Key takeaways:
- The current Omicron wave appears to be at least as big as the one six months ago, at least in our social group
- Nearly all survey respondents were fully vaccinated prior to Omicron, and nearly all did not get COVID prior to Omicron. Most respondents were between the ages of 25 and 45.
- The average respondent who caught Omicron was stuck in bed for about 2 days, and not back to full productivity for about 5 days. Long COVID symptoms were noted by a small proportion of respondents.
- A large fraction of respondents who caught Omicron caught it at indoor private gatherings or events
- Field evidence of the benefit of rapid testing at events suggests some benefit, but the evidence is limited and conflicting, and rapid testing definitely isn't 100% effective at preventing transmission at events.
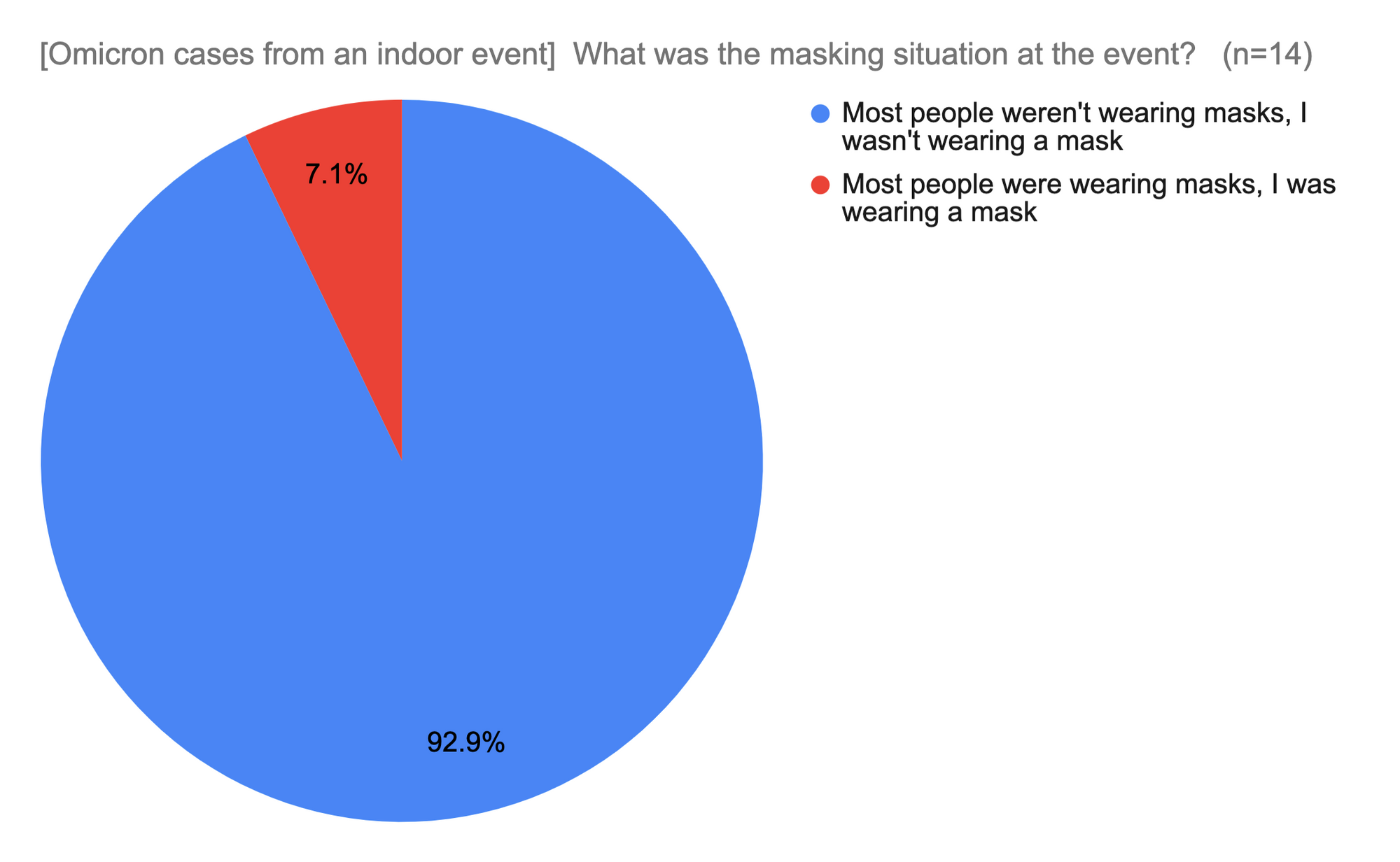
- Catching Omicron when masked is rare, but does happen
Motivation
My social group, like other social groups all around the world, has grappled with how much effort to put into COVID precautions. In general we've tried to be evidence-based with whatever evidence was available at the time, and tried to keep our risk low while still living our lives as much as possible given that constraint. We did really well at this, with only a small fraction of us getting COVID prior to Omicron. However, as vaccines, rapid tests, and treatments have become available, we've looked to figure out how seriously to continue to take COVID.
A significant number of people in our group caught COVID during the first Omicron wave in Dec 2021 - Feb 2022, but then again, a large fraction of America caught it during the same period. We figured after this, COVID was likely over, as our country appeared to have reached herd immunity.
In late April 2022, a curious thing happened – a startlingly large number of people in our friend group started reporting getting COVID. Local caseload was still very low. I couldn't tell if this was a broader phenomenon being hidden by changes in case reporting or simply a local mini-outbreak in our social group. Furthermore, I couldn't tell how much to worry about it.
I decided to do a survey of my friends on Facebook to learn what their experience of Omicron had been like. I hoped the data would have a large enough sample size to deliver relevant results while being local enough to me to provide useful data.
Making surveys is a tradeoff between asking enough questions to be able to do a good statistical analysis versus making the survey so long that you don't get a lot of respondents. In general I aimed for a shorter survey, and ended up with 83 responses.
I will admit this isn't rigorous science, but it's designed to do a decent job of giving personally relevant answers to questions not covered by national-scale data while being more useful than anecdotes like "My friend Eddie had it and it wasn't that bad." Large effect sizes are often easy to see even if techniques are less rigorous. I should note that the results here are particular to my social group, and they may or may not apply to your social group, but the general principle of doing a survey to learn this sort of thing could apply to your situation.
In general I wanted to understand (1) whether we were indeed having another big outbreak, (2) what getting Omicron was like, and (3) what precautions people in our social group were taking, and what impact it was having. Here's what I learned:
Who are these people anyway?
A good fraction of the people who would have seen the survey live in the San Francisco bay area and other major cities in the US and internationally. A good fraction of them are in various white-collar tech (software, hardware, biotech) jobs, but there's also a mix of other professions as well. The survey was served up in the Facebook newsfeed, so the people who completed it were people who cared enough to do a short survey on COVID. I tried to make the description as minimal as possible so as to not bias the respondents.
About 80% of survey respondents were between the ages of 25 and 45, with the rest being older than 45.
Very few of the respondents caught COVID during the pre-Omicron period, which I defined as before Dec 15, 2021.
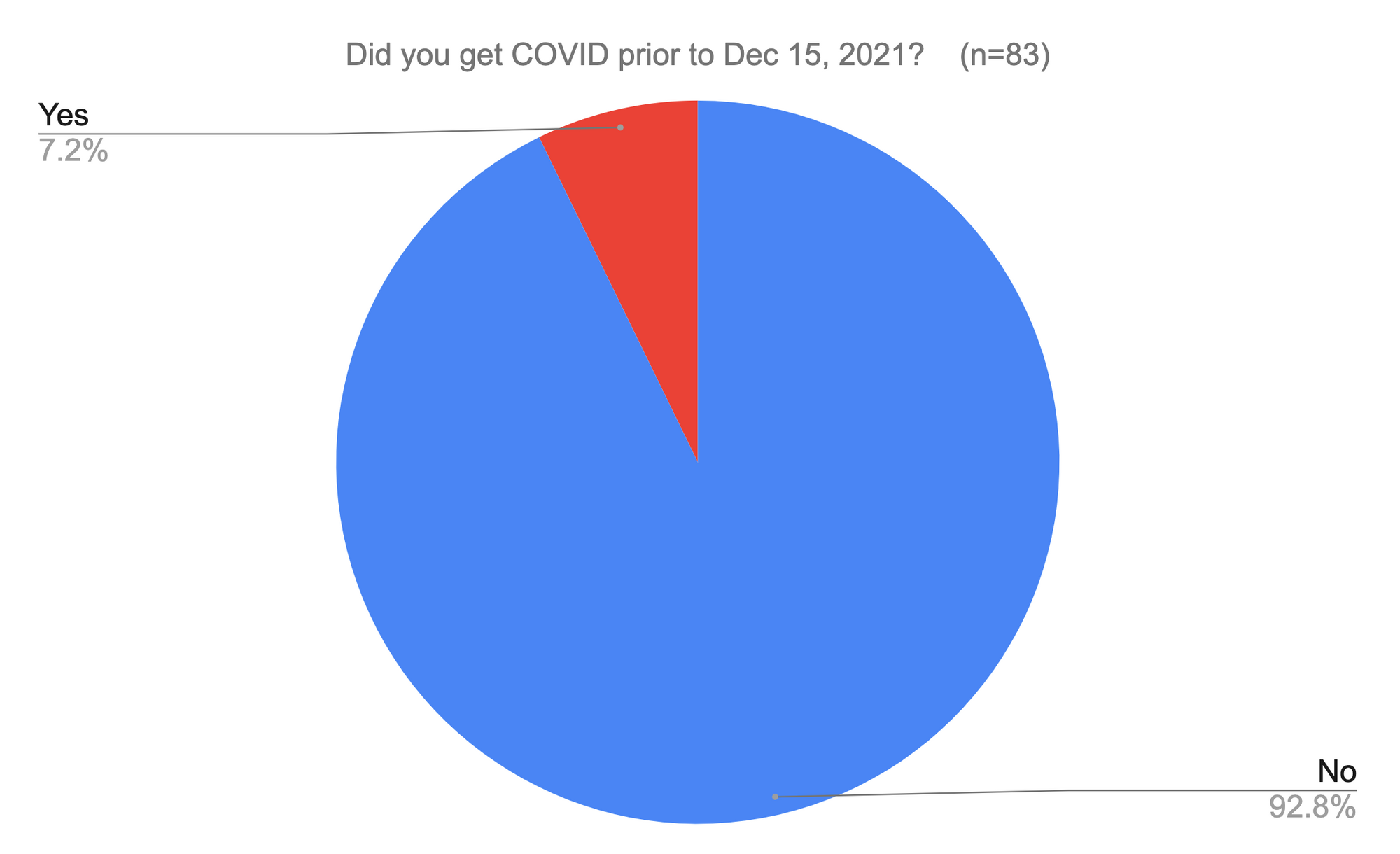
About 15% of Americans officially got COVID during the same period, with the real number likely being significantly higher. Tests were so hard to come by during the first wave that people were rarely tested unless they were getting admitted to the hospital (and even then, sometimes not).
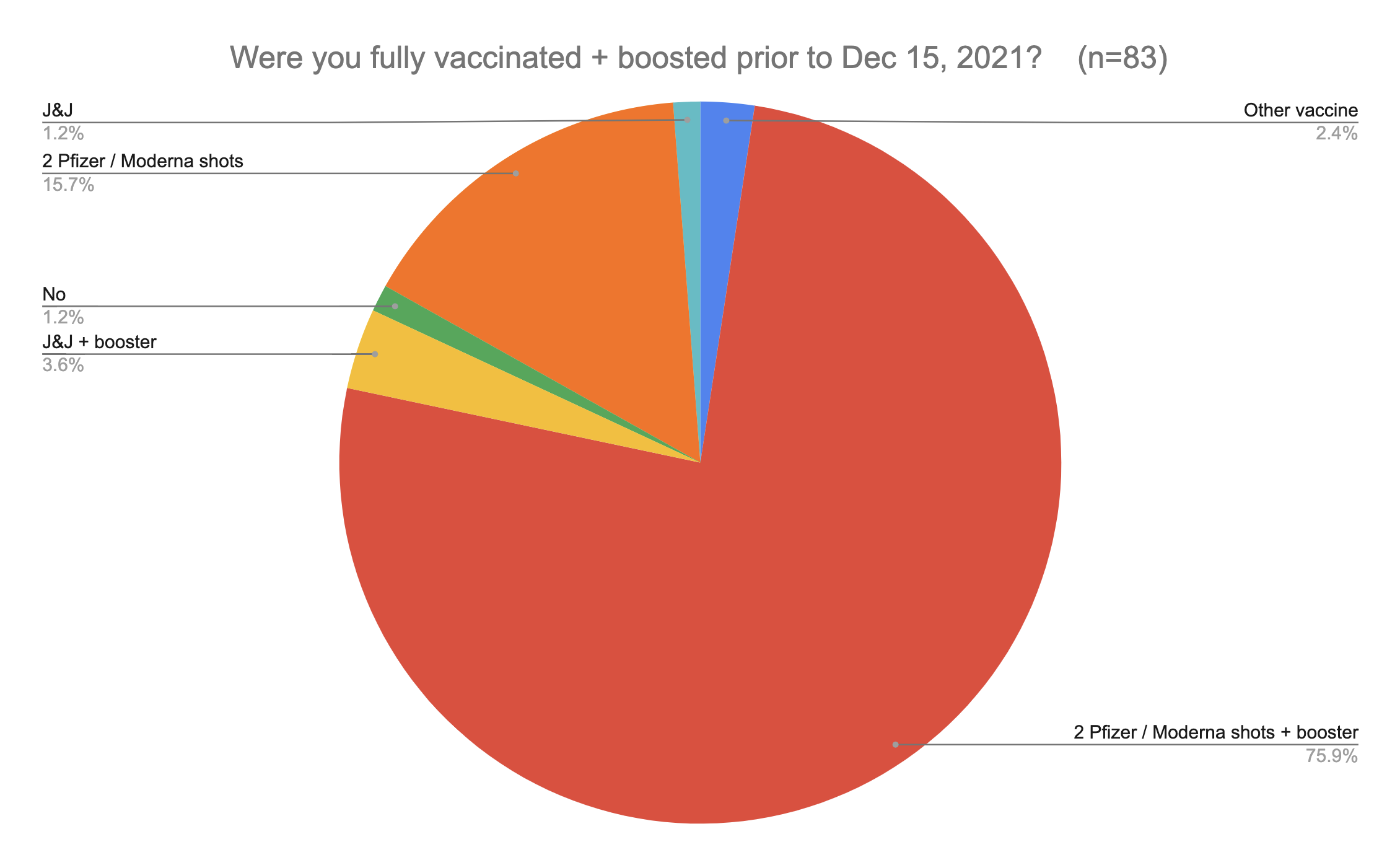
Almost everyone who completed the survey was vaccinated.
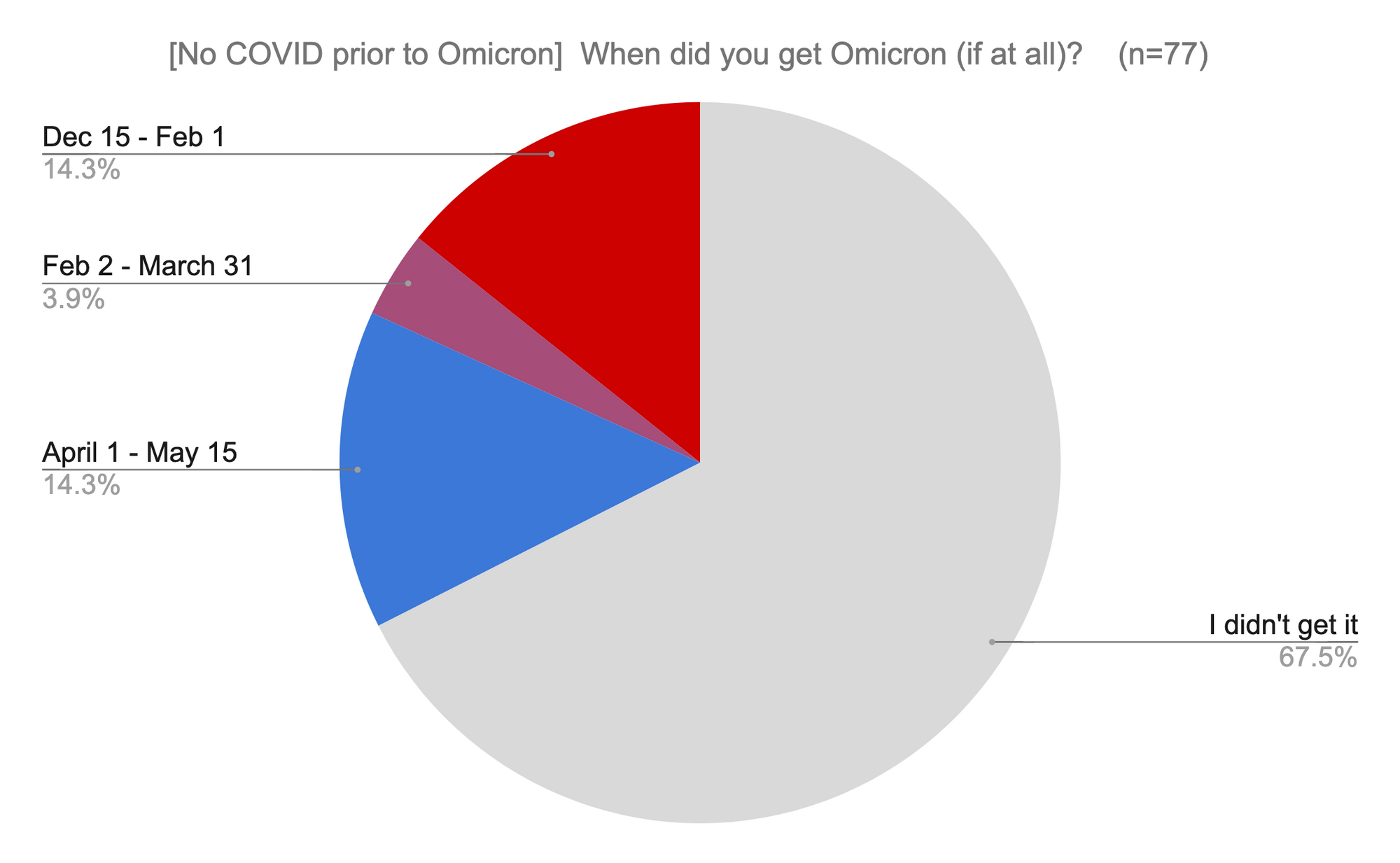
Are we indeed having another huge outbreak?
Official city case counts (see below) as well as state and national data definitely don't seem to think so. However, at this point many groups are no longer bothering to test or report their cases, so it's possible there is significant underreporting.
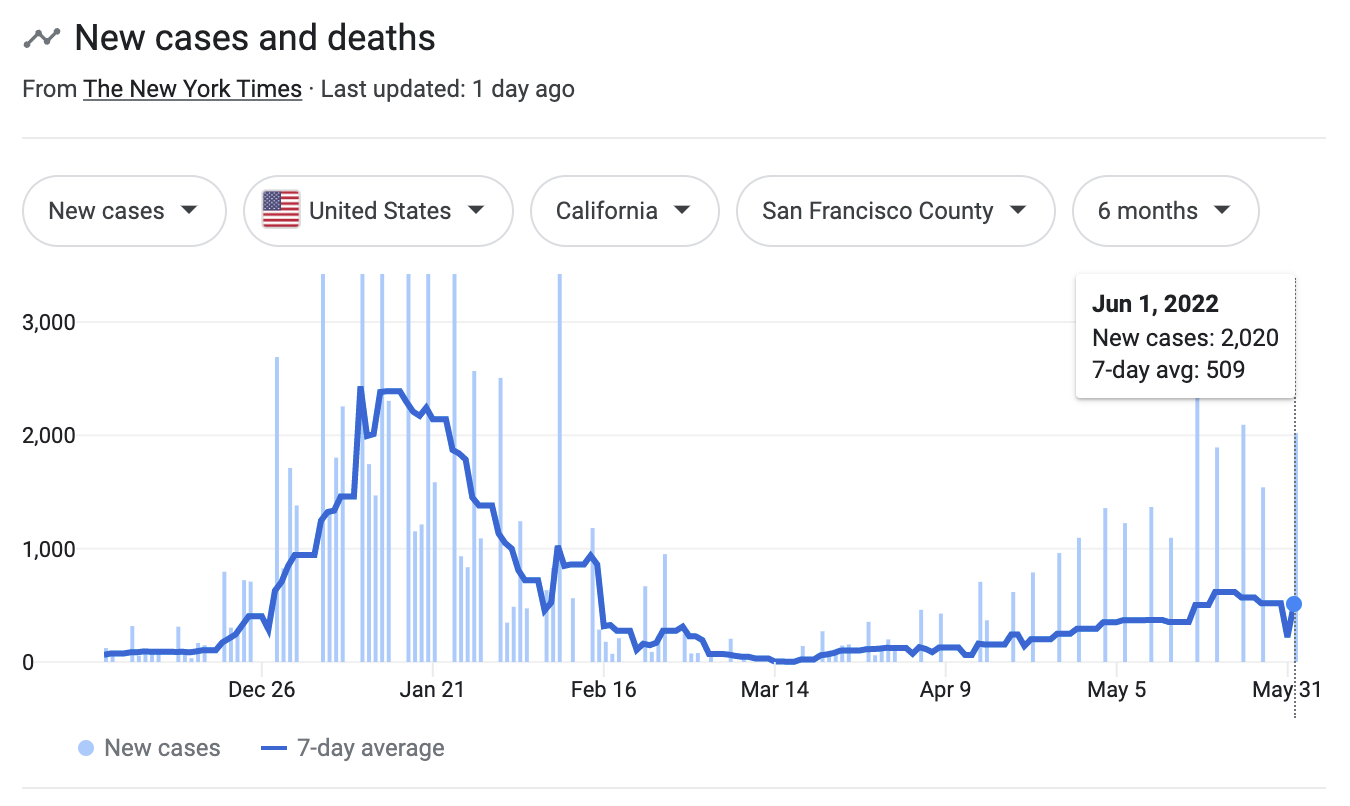
My friend group is definitely having an outbreak though. The same number of people got it during the last month and a half as did during the first Omicron wave in December 15, 2021 - Feb 1, 2022.
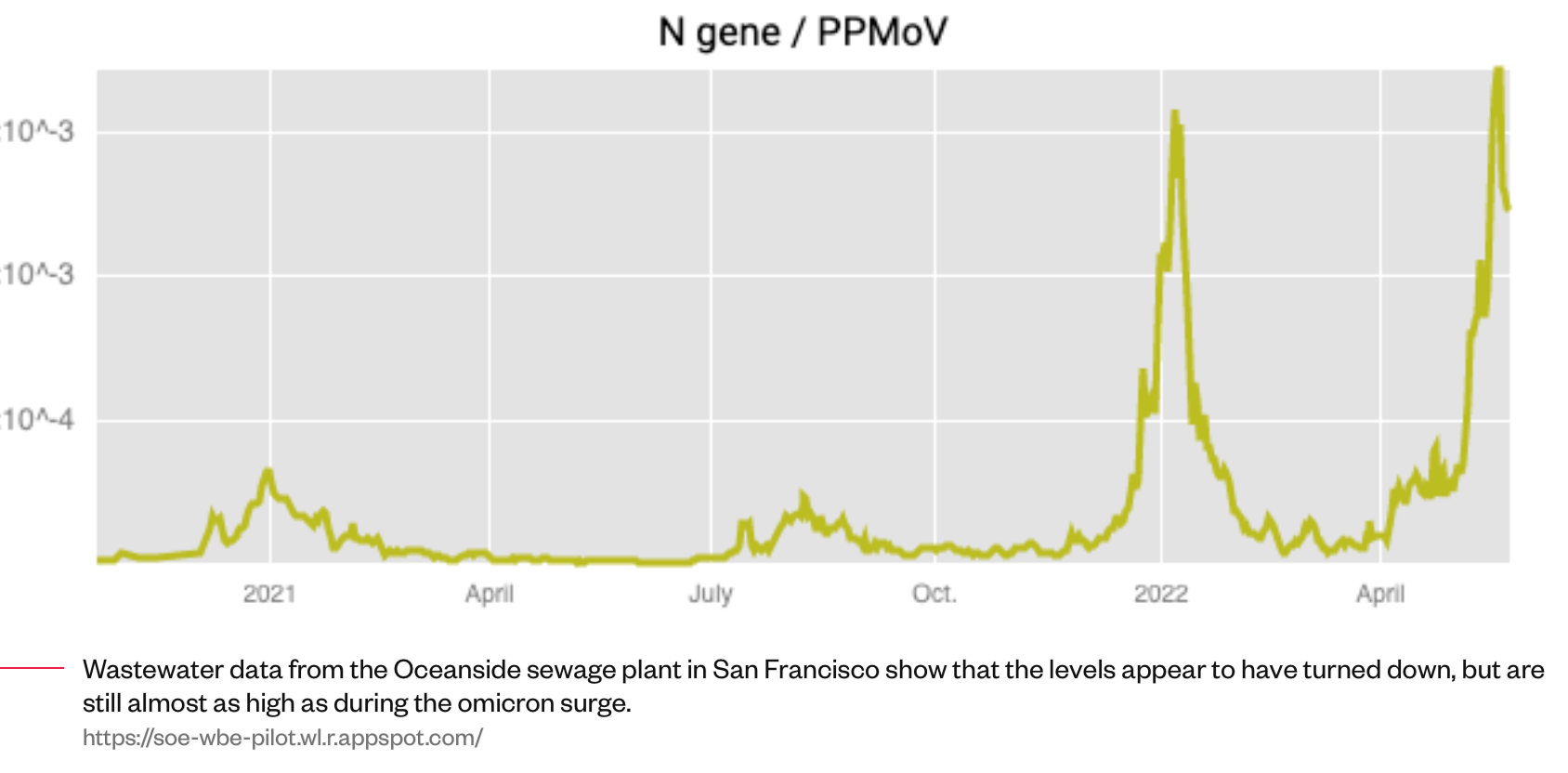
It's still unclear if this is just happening in our social group, but there's some evidence it's not. Wastewater genetic screening data from SF's treatment plant suggests that the current amount of COVID genetic material in sewage is as high as it was during the first Omicron peak. However, wastewater data is not that accurate in comparing across longer time intervals as different variants have different viral loads, and the current Omicron variants are different from the ones six months ago.
What's it like to get Omicron?
I asked survey respondents for their experience of Omicron.
For most people, the experience was significantly unpleasant, but not too bad. The average respondent was stuck in bed for about two days and had reduced productivity for about five.
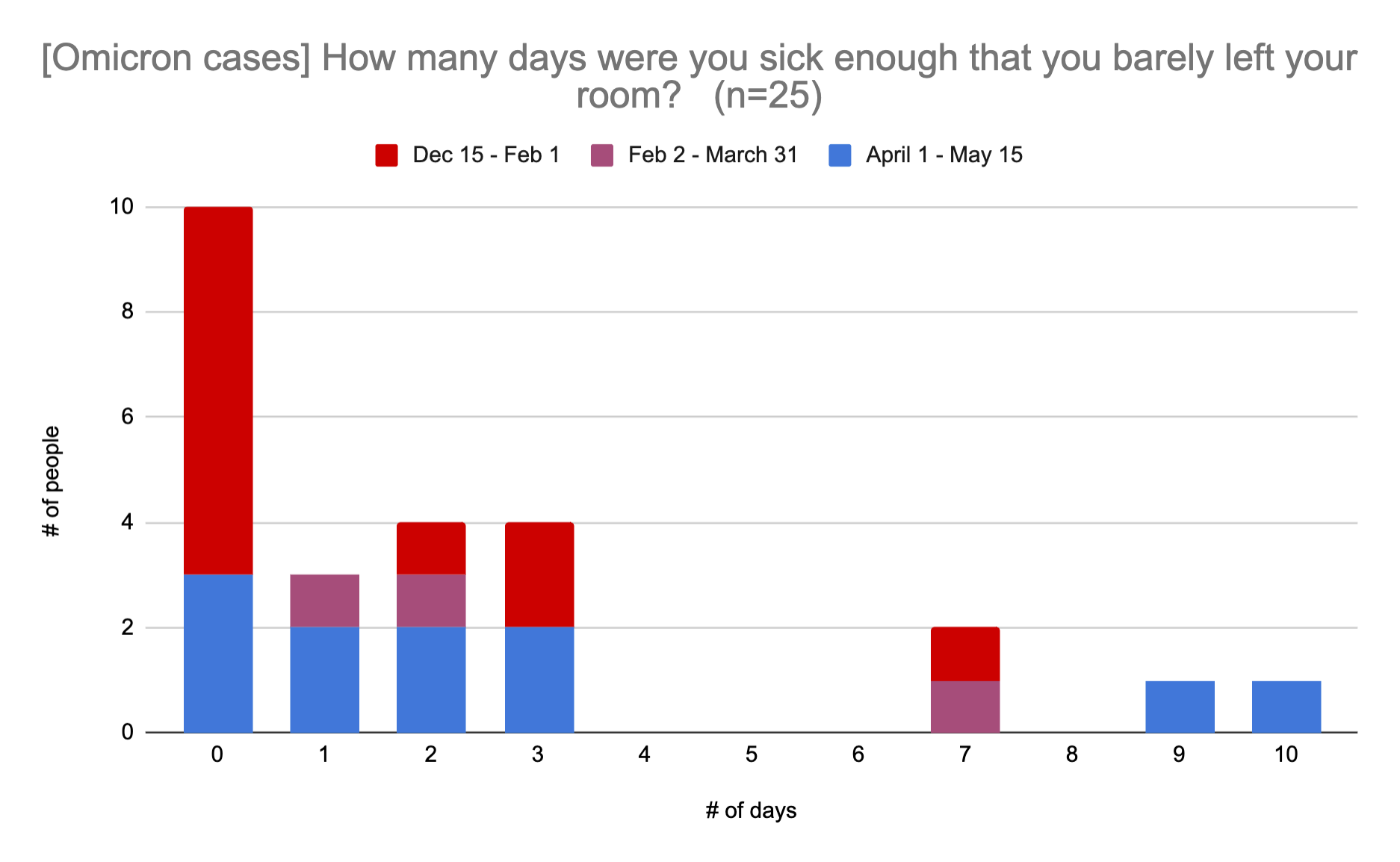
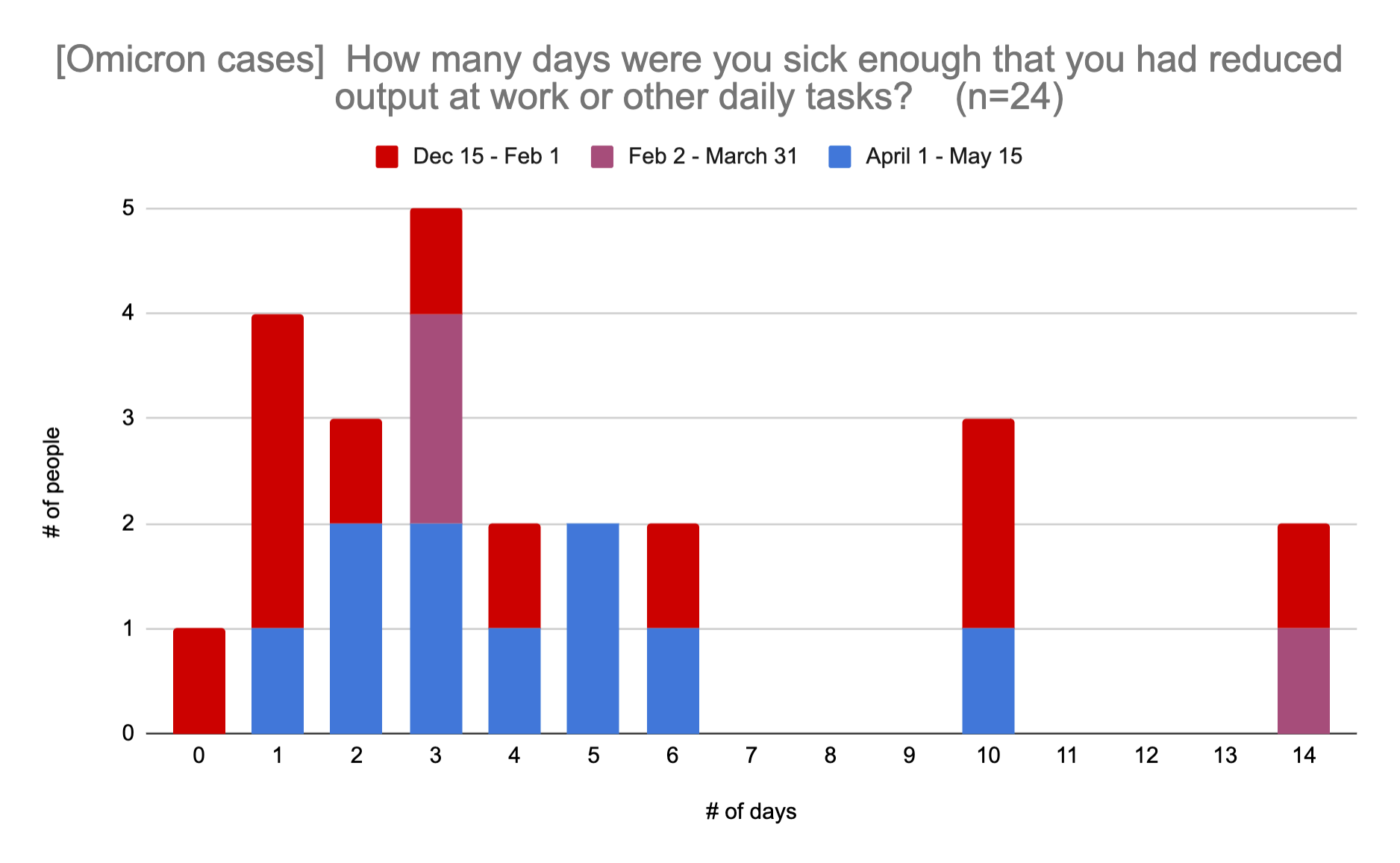
Everyone needs to make their own call on whether their current level of COVID precautions is worth some chance of preventing some chance of a few days stuck in bed. However, the combination of vaccines, early detection through rapid testing, and readily available Paxlovid seems to make the disease not too bad on average.
I also asked people how much money they would have paid to have not had COVID, and the average was $446, with the minimum being $0 and the maximum being $2000. Obviously this would be different for people in different economic situations, but I found the quantification interesting (and the numbers surprisingly low).
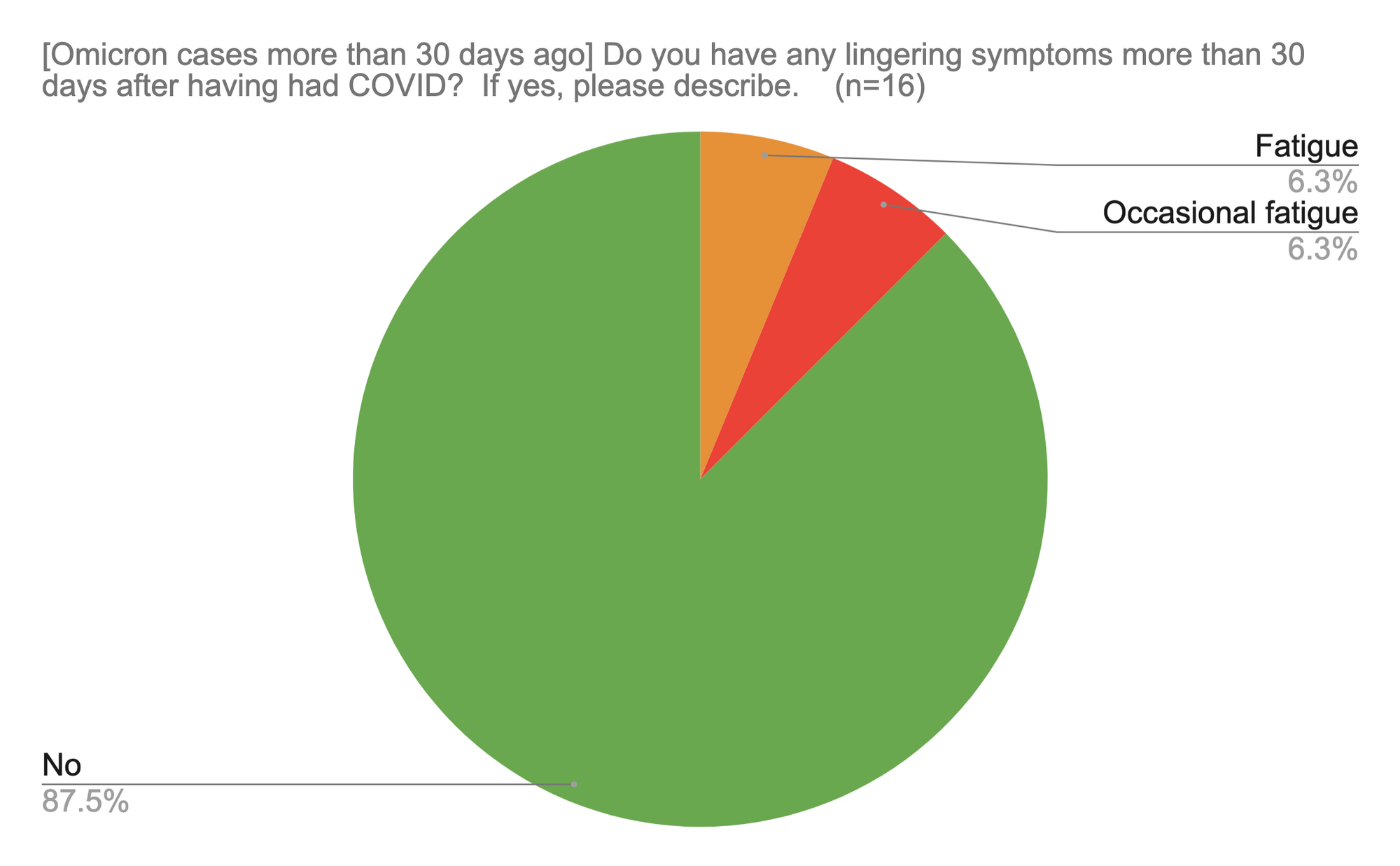
The one wildcard is long COVID, which has proven to be extremely hard to pin down. A couple of people reported still having some fatigue more than 30 days after getting Omicron. I unfortunately don't have useful context on those people, as the survey did not go into other health conditions. There's a big and messy set of studies on long COVID that's almost always out of date with the latest variant and (since we don't have a time machine) doesn't offer any insight into the incidence of long COVID with Omicron past 6 months.
What precautions are people taking, and what effect is it having?
It's interesting to look at where people caught Omicron.
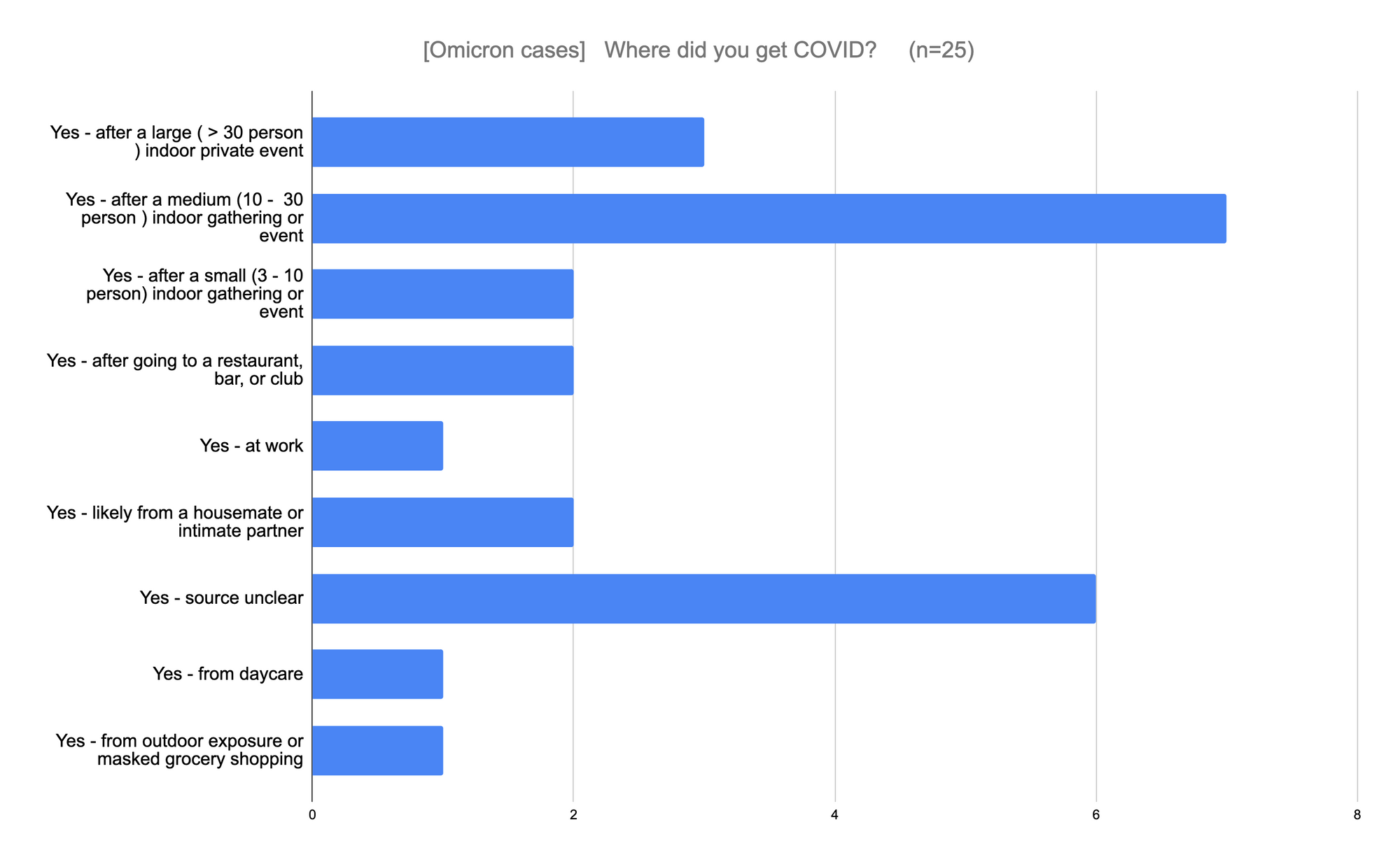
Medium-sized events were the most common source of infections. It's important to note that we don't know how much people are altering their behavior because of COVID precautions, nor the base rate of their time spent in these various environments.
We can see that there are significant differences in the behavior of people who did vs didn't catch Omicron:
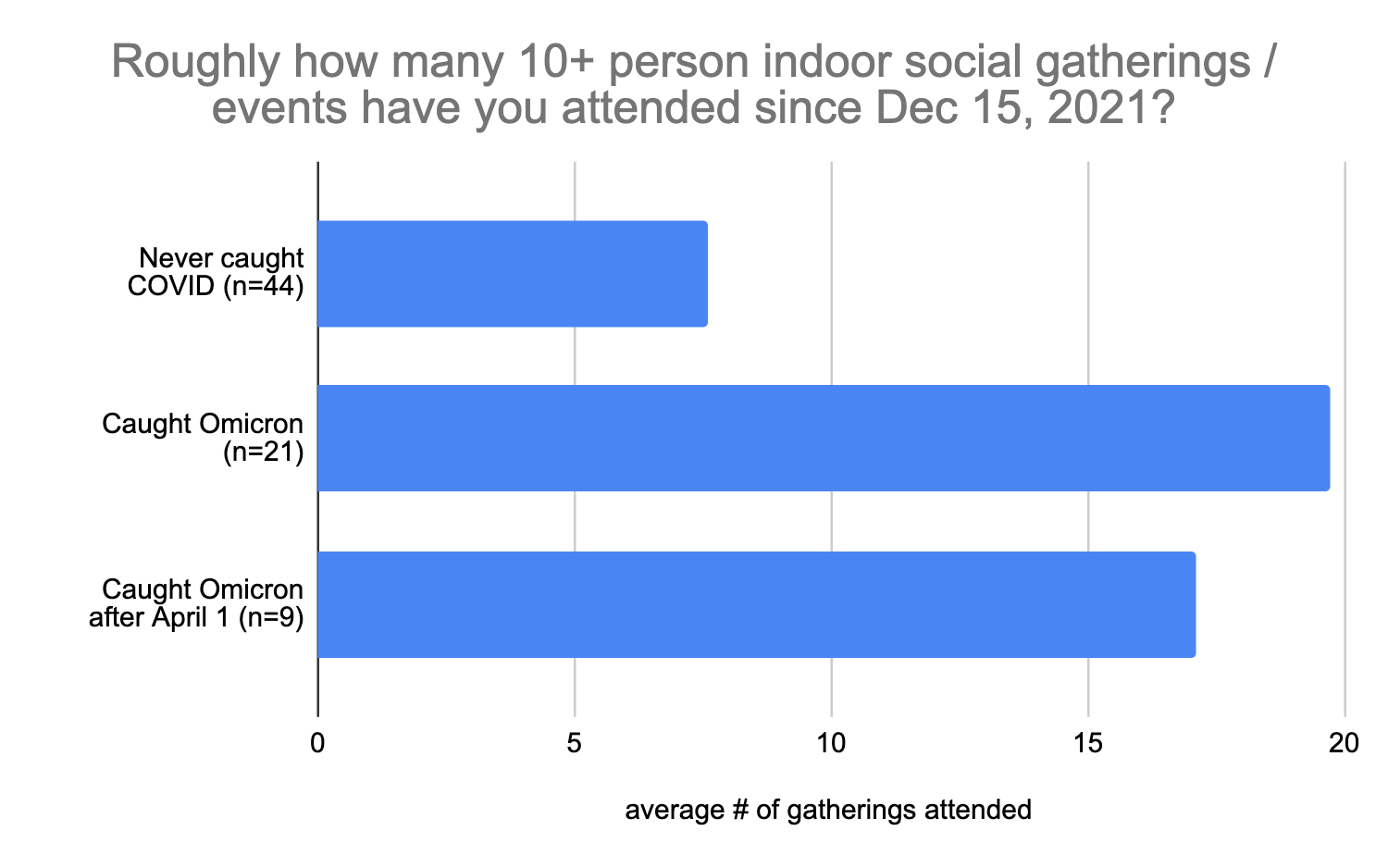
In a not-surprising-at-all result, people who caught Omicron were going to substantially more events, though interestingly the variance on this was quite high, with a person who never caught COVID reporting attending over 100 events. It would not surprise me if some people have a very high genetic resistance to catching COVID. (These numbers were a bit difficult to work with as multiple people gave vague estimates like "a ton". I substituted an exact number when people gave a precise range, but not when they used a qualitative description or something like "more than X".) I included people who caught Omicron after April 1 as a separate category as the people who caught Omicron during the first wave likely took few precautions after recovering, and I wanted to look at behavior prior to catching COVID.
Another area of interest is whether or how much rapid testing or PCR testing at the door to an event prevents infections at the event. In general, people who caught Omicron also tended to attend a greater proportion of events without testing requirements.
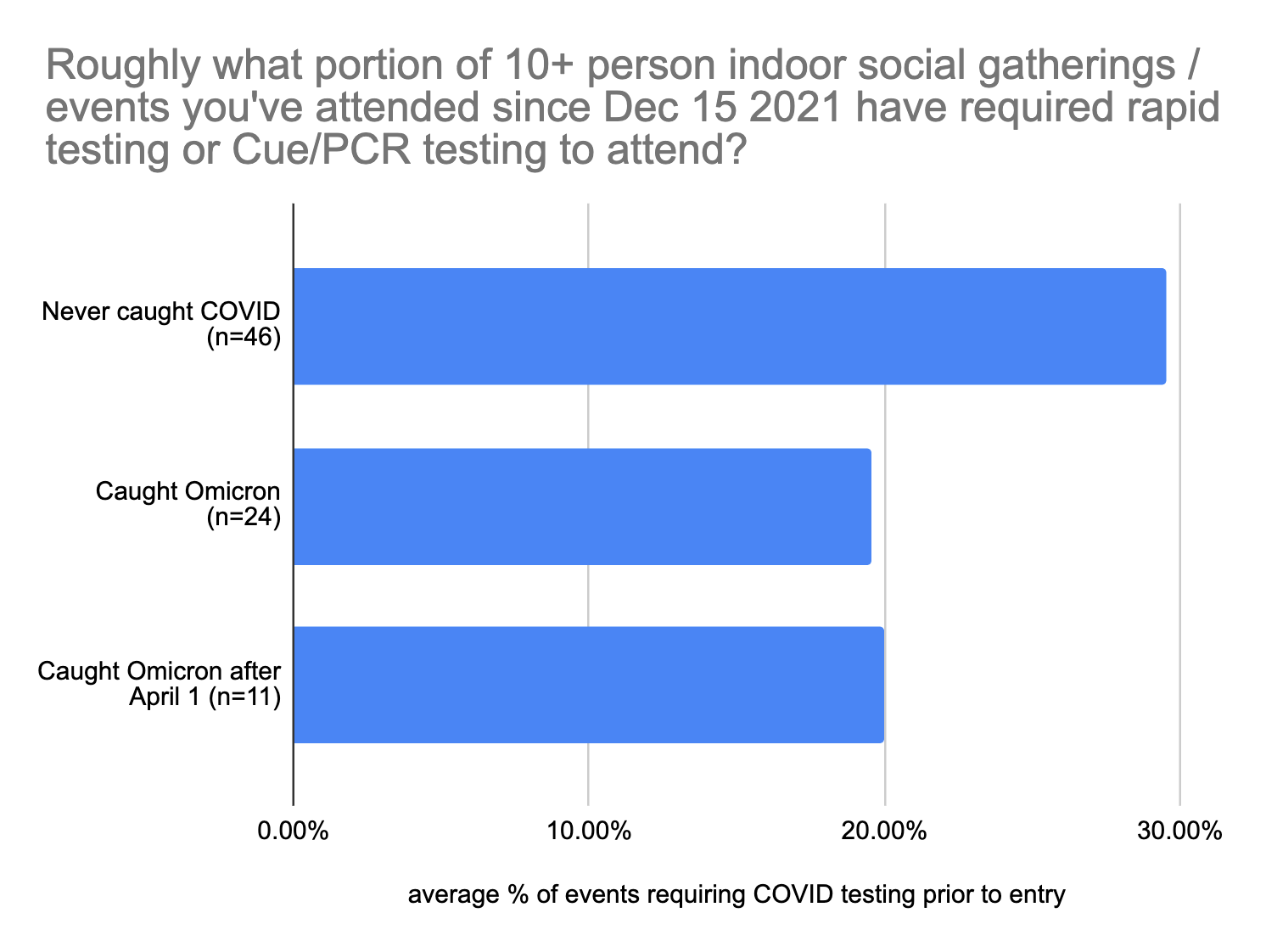
However, it's possible that this effect might be illusory – it's conceivable that testing at the door is just security theater, and people who are taking other (effective) precautions are more likely to favor events that have testing at the door.
If we look at the composition of the cases where people caught Omicron at an event, the portion that required testing to get in (33%, or 22% if you only count rigorously enforced testing) is higher than the proportion of events that these people reported attending that required testing to get in (20%).
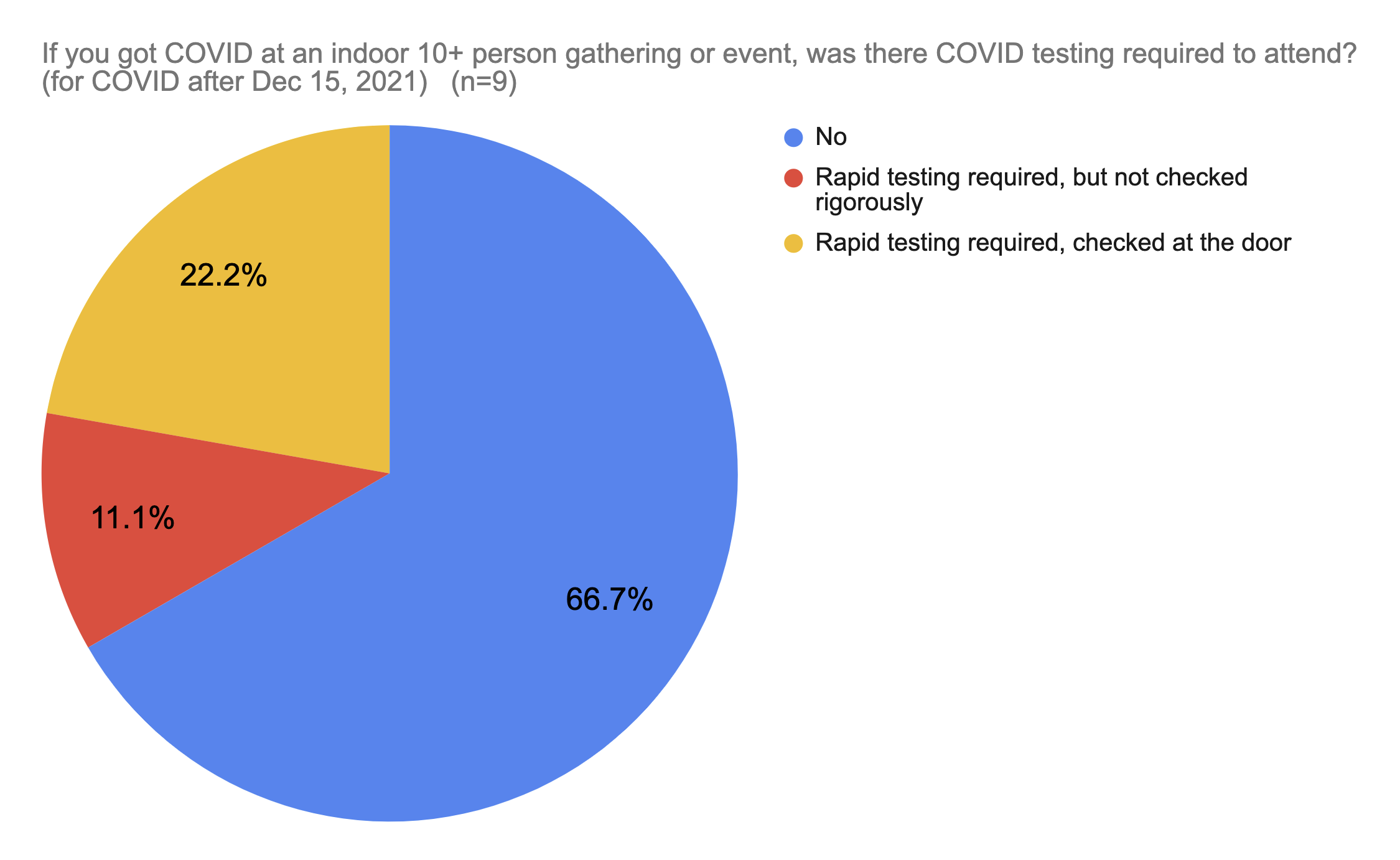
This result does not show a benefit to testing at the event, assuming all events are equal. However, the sample size here is very small, so it's risky to draw premature conclusions from it. Also, one of the people who caught COVID at an event with required testing at the door said it was a very intimate event that involved a lot of exchange of fluids, and thus it was an extra-high-risk event where even lower caseloads would have been prohibitive.
The biological evidence shows some support for the value of rapid testing. Contagion tends to vary with viral load, and viral load varies a lot, over several orders of magnitude.
Here's a pre-Omicron graph of the reliability of rapid antigen testing at catching cases of viral loads. Rapid antigen tests are very good at detecting high-contagion high-viral-load people, and not very good at detecting low-contagion low-viral-load people.
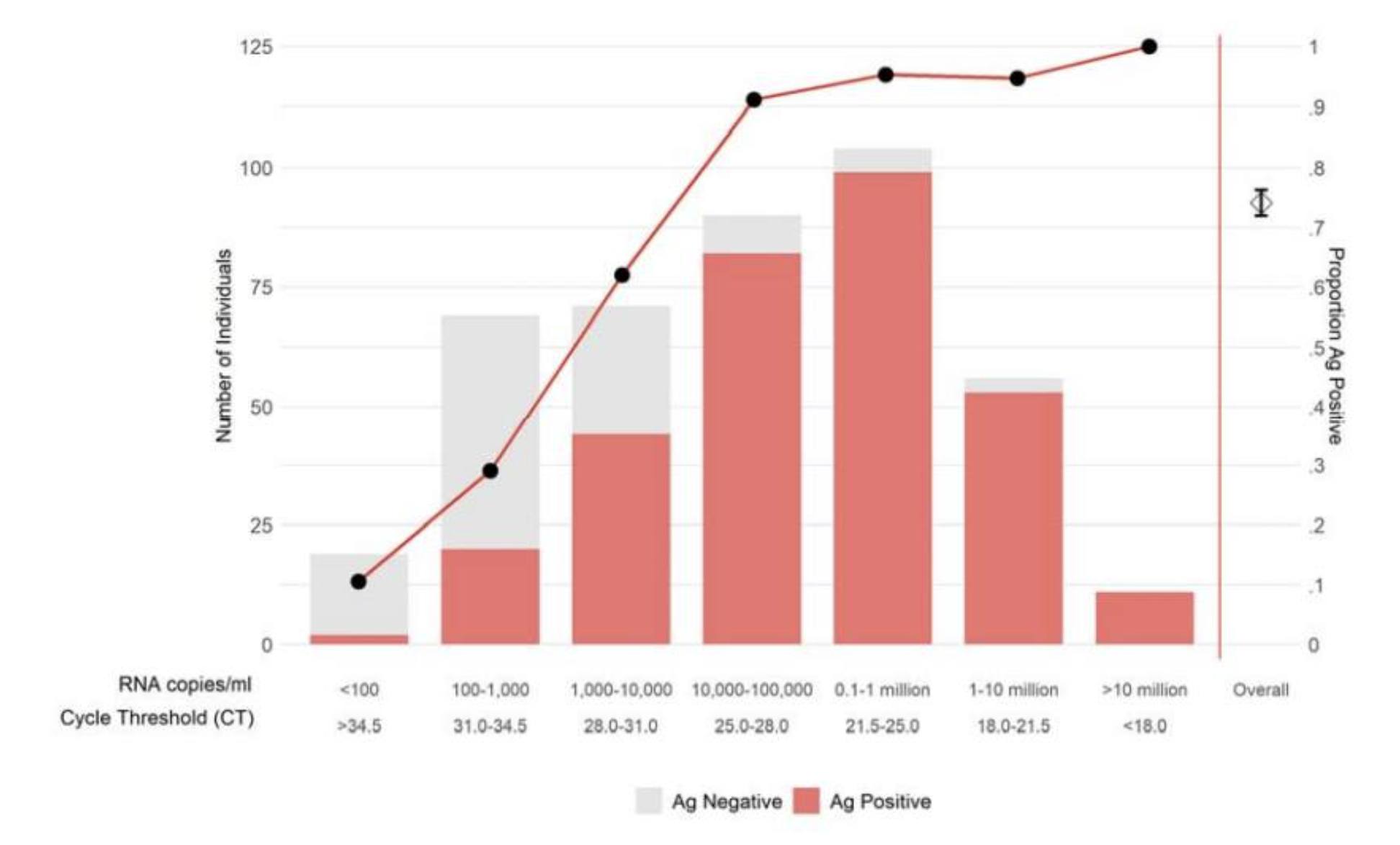
With a low viral load, you'd have to kiss someone to transmit it to them, whereas with a very high viral load, you could give it to them from across the room simply by breathing for a few minutes. Thus, rapid antigen testing should theoretically be very good at detecting superspreaders, but much less good at detecting people who are mildly contagious.
The actual benefit of rapid antigen testing at the door for an indoor event thus likely depends on the density and intimacy of the event. However, rapid antigen testing is clearly not 100% effective. For high risk events, testing with PCR-grade Cue tests would do a very good job of detecting COVID cases, even ones with low viral loads. I'm aware of one event organizer who required PCR testing for a 1,500 person indoor event in February 2022, and did not get any reports of people contracting COVID at the event.
Meanwhile, a few days after putting out the survey, our nanny tested positive upon entry to our house, with a very high viral load, despite being completely asymptomatic. It's likely that the daily rapid testing we do for everyone who enters the house prevented most of our family (baby included) from getting COVID.

It's likely that rapid testing at the door is at least somewhat effective at preventing infections, though the data is murky on actually how effective it is. I'd love to have had a clearer conclusion on this. Personally, we'll keep doing rapid-testing for indoor unmasked events we host while the caseload remains high.
Finally, it appears that while transmission of COVID at masked events is rare, it did happen on at least one occasion. I unfortunately did not collect survey data on the base rate of what portion of events people attended were mostly-masked or on the quality of masks used. I continue to believe that using a good quality mask (KN95 or better) when in indoor settings is a great way of keeping COVID risk minimal.
Conclusions
Portions of our country forgot COVID existed a long time ago. Other people are still wearing masks outdoors when walking down a not-so-crowded sidewalk. People's risk tolerance still seems to vary on the order of tens of thousands.
The acute risk to catching COVID has fallen very substantially, to the point where it is similar to other flu strains.
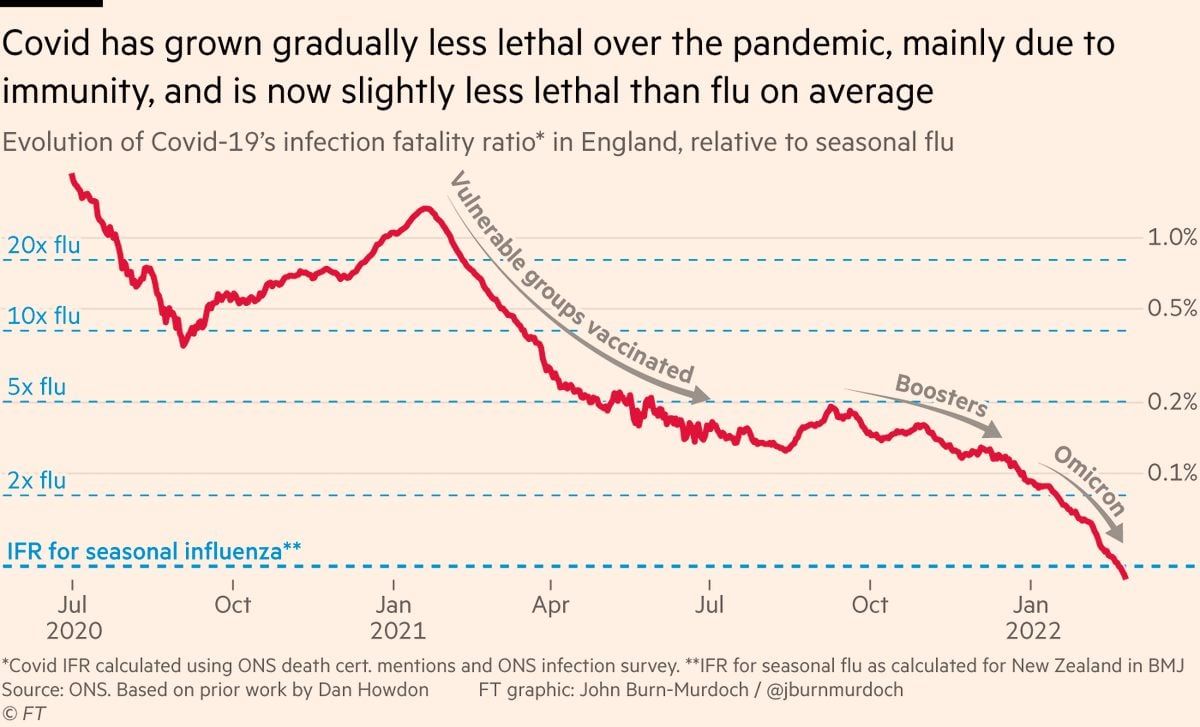
I think that for the purpose of avoiding acute COVID alone, fewer precautions are merited these days. My friend group's experience shows that the illness is a pain, but is not that much worse than other illnesses we regularly encounter. Thanks again to the developers of the vaccines, rapid tests, and Paxlovid for making that possible.
Long COVID remains an unknown risk, a low (probably single digit percentage) probability of a long-term negative consequence, and this still forms the bulk of my remaining concern around catching COVID. I last did a deep dive into this several months ago, and clear answers were very hard to come by. Definitions of long COVID vary substantially in terms of time frame, persistence, and severity, and it's often hard to establish clear causality from acute COVID to a permanent debilitating condition, especially in a population of people that has some who already have chronic hard-to-pin-down health conditions.
There's also a reasonable argument that COVID will be endemic at this point, and given the relaxation of precautions and the continued waves of infection two years in, this seems very likely. In that case, is it worth taking precautions at all if you're just going to get it at some point? Perhaps. It depends on your situation and whether high risk people live with you. Each wave of infections that you manage to avoid gives the medical establishment more time to develop better protocols and treatments, but it also is another few months of events and social gatherings that you partially miss out on.
I'm personally still being more careful during the periods of time when local caseload appears high, limiting indoor dining to special occasions, strongly encouraging testing at indoor unmasked events, and masking up in other indoor situations with large groups of unmasked people unless it's a special occasion that merits the additional risk. I'm still missing out on a lot of events, and that makes me a bit sad. Hopefully it's worth the tradeoff of making it a couple of percent less likely that I end up with some long-term difficult-to-pin-down health issue. During periods of lower caseload I'm taking fewer to no precautions.
I would love to live in a world where everyone takes a two-minute test in the morning for a variety of contagious diseases, and then takes precautions avoids events that day if they test positive or are showing symptoms. It would be part of a morning routine like teeth-brushing. I've enjoyed barely getting sick at all over the last couple of years, and would love to see a world where people rarely get each other sick. However, I'm guessing that the tech to make this possible and extremely inexpensive is still a few years away, and getting high social cooperation around this would be really hard, as the contagious-but-not-too-sick person often benefits from getting on that airplane or going to that party. Hopefully we can at least instill a new norm in our social circle of not coming to events if you're sick so as to not get anyone else sick.
