
If you have a mask already, wear it. You can sterilize and re-use it.
If you don’t have a mask, improvise one. You can sterilize and re-use it.
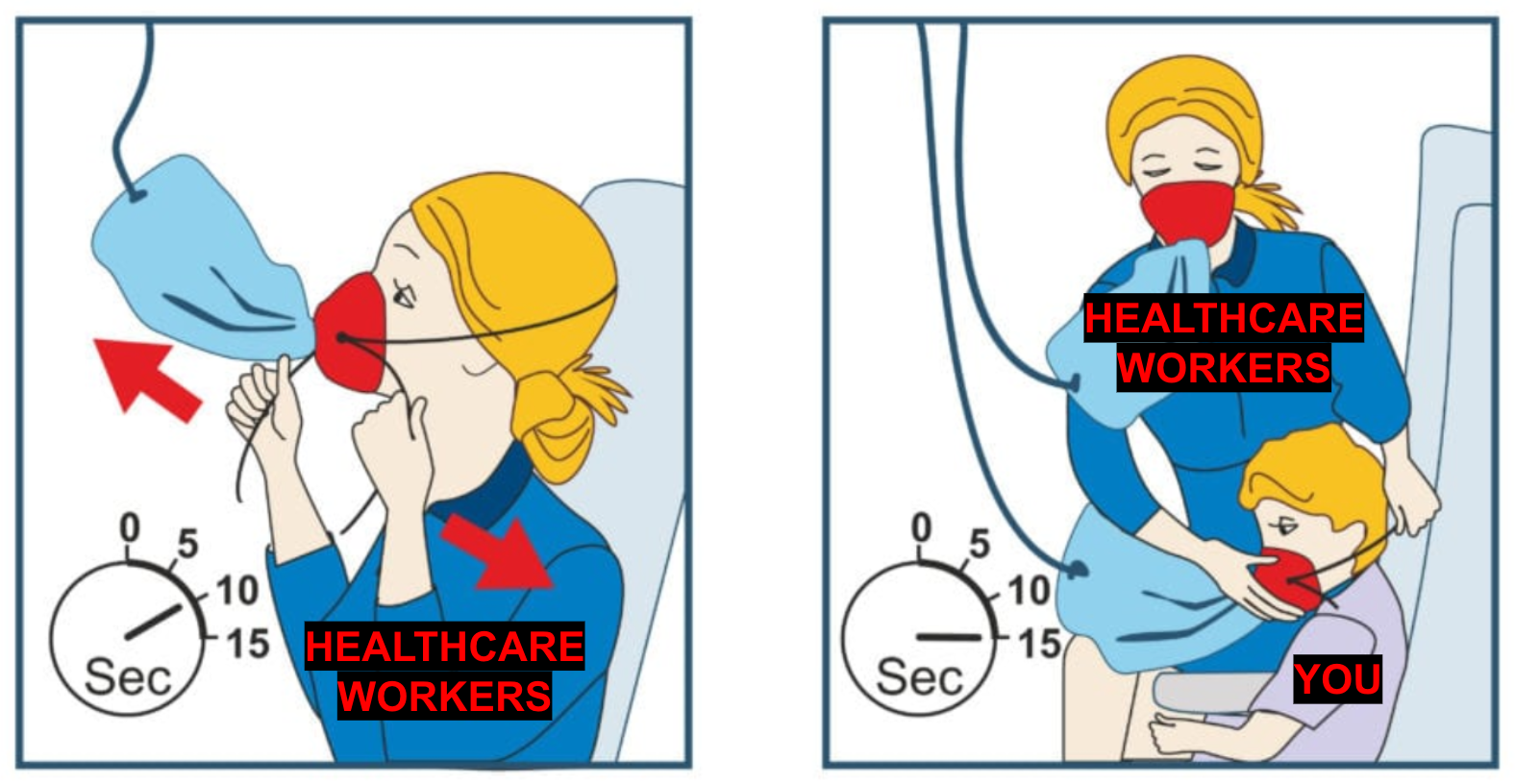
If you have a lot of masks in their original packaging, donate them to a local hospital. Healthcare workers are at much greater risk than you are of getting infected, and there are shortages. You also want them to be healthy so they can take care of you. It’s like that part of the airline safety video where they tell you to affix your own mask before assisting your child, except that doctors and nurses are you, and you are the child. Here’s a nationwide (US) site listing locations for Personal Protective Equipment donations.
There are many types of masks with different levels of filtration ability. A P100 respirator is better than a N95 respirator, which is better than a surgical mask, which is better than a scarf or pillowcase. However, all of these masks are significantly better than nothing. Don’t despair if you don’t have the best mask. Make do with what you have. Try to get it to fit as well as possible. Disinfect it after each use so you can reuse it.

Do Masks Work?
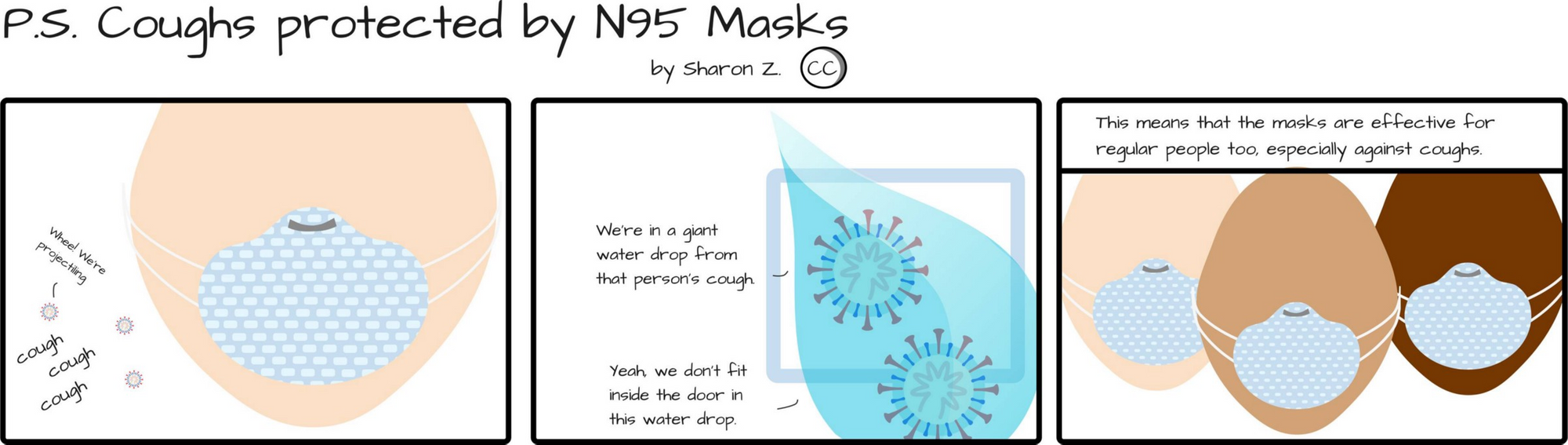
Aside from washing your hands regularly, avoiding physical touch, not gathering in large groups, and isolating yourself when you’re sick, wearing a mask could be one of the most effective things you can personally do to prevent the spread of COVID-19. It could reduce your chance of catching COVID-19 as well as your chance of spreading it if you’re sick or asymptomatically infected.
In addition to providing some degree of protection against inhaling or spreading droplets with virus in them, masks prevent you from touching the mucous membranes of your face with dirty and possibly infected hands when you’re out in public.
How do we know if masks work? Here are three ways:
- Test in a field setting by running randomized controlled trials during regular influenza season.
- Test at mass scale during a pandemic by looking at epidemiological data.
- Test in a lab setting by making physical measurements of porosity.
Each method of study carries different limitations.
Let’s start with the field trials. There have been many studies on respirators and masks in healthcare settings as well as home settings in which a family member is sick. If you want to dive into the details, this review of the literature is a good place to start. At a high level, studies on the protectiveness of masks in real-world settings are complicated to do and confounded by other factors, but there is strong evidence that masks are useful in healthcare settings and decent evidence that masks are useful in home settings. From this, you can extrapolate that masks would likely be helpful in a pandemic setting.
Here’s some more detail on this extrapolation: Home setting studies are particularly difficult to show effectiveness. These studies require participants to wear masks at all times while at home with a sick relative. Relatively few people adhere to this protocol because it’s tiring to wear a mask for the whole day. However, in a pandemic setting, you’re only wearing a mask for a few hours while out shopping or at the office. Separately, people are much more afraid of catching a disease during a pandemic than they are afraid of catching a regular flu during a study. Thus, I’d expect that people would wear masks much more reliably in a pandemic setting than in a home study setting. This means the results of mask use in a pandemic setting will likely be better than they are in a home setting, and these results were already decently good in a home setting.
There’s very little research on cloth masks in either healthcare or pandemic settings as almost everyone uses N95 or surgical masks when they’re available. To get a sense of their effectiveness, we’ll have to rely on direct analysis of their ability to filter droplets and particles, which is covered later in this essay.
The Big Picture
To get another sense of how effective masks might be, let’s look at comparisons between nations that are and aren’t encouraging the public wearing masks during the COVID-19 pandemic.
Nearly every Asian public health ministry recommends that people wear masks in public, especially during the winter flu season. Japan, Hong Kong, South Korea, and Taiwan all recommend wearing masks, and all of these countries have been effective in slowing the spread of COVID-19 within their borders without having to resort to Wuhan-style lockdowns.

This is such a huge deal that it bears repeating. Daily life in Japan, Hong Kong, South Korea and Taiwan is only slightly affected. Some large gatherings are prohibited and some schools are closed, but life on the street is only lightly affected. Stores, restaurants, and most other businesses are open. What do these countries have in common? They all were affected by the SARS epidemic in 2003. When news of COVID-19 broke, everyone put on masks and started sanitizing or washing their hands every time they entered an office or restaurant. Taiwan in particular had an almost immediate response that involved nationwide requisition and distribution of masks to hospitals and to the general public almost as soon as the Wuhan lockdown happened. Taiwan managed to cap its total cases at 169 (as of 3/22/20) despite the enormous number of people traveling daily to and from China when the outbreak occurred.
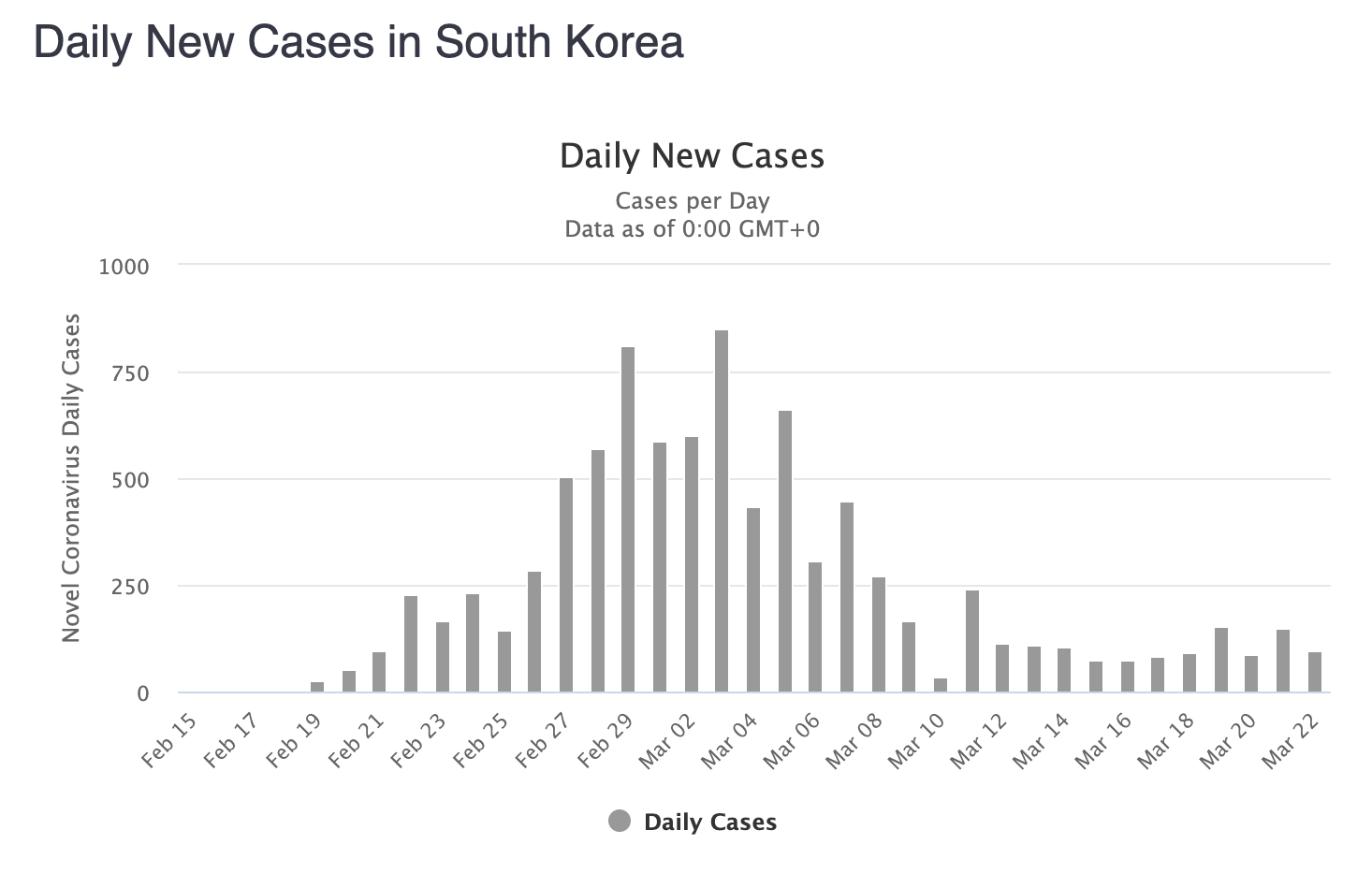
Some of these countries are also doing some other things that are quite effective — South Korea in particular is doing an excellent job of tracing the contacts of everyone who might have been infected and aggressively testing them to encircle any outbreaks that are happening. This is undoubtedly vital to controlling the spread of the disease.
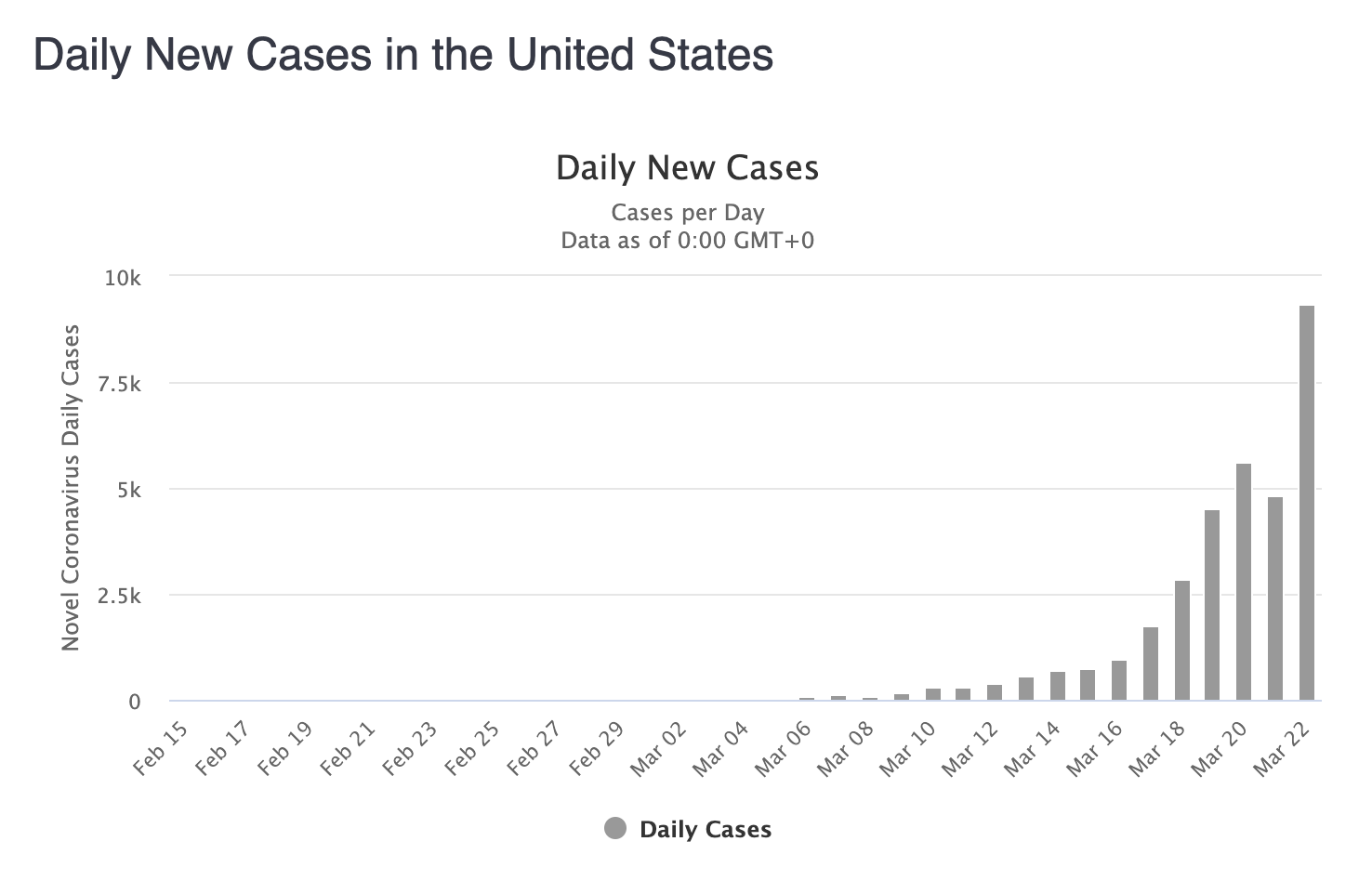
Let’s compare South Korea to the US.
It’s easy to tell yourself just-so stories about why your favorite factor is the cause of something when in fact it was mainly caused by something else. Maybe these countries are successful mostly due to aggressive testing and contact tracing. However, there’s an interesting counterexample that helps put this to the test. Japan is actually being inexplicably lazy about contact tracing and is only testing reactively, waiting for people to get sick first. Even so, their number of new daily cases looks like this:
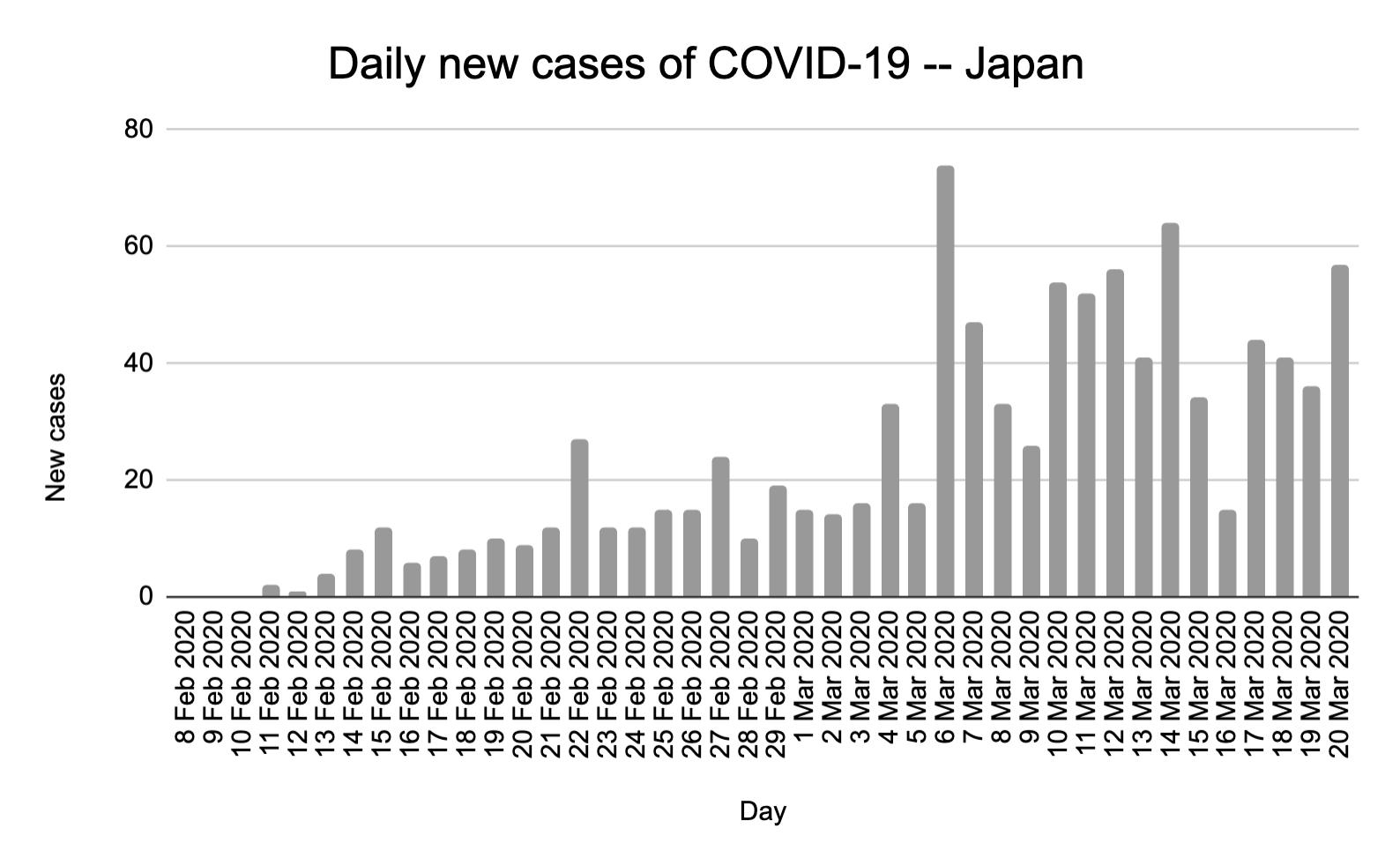
It’s going up, but it’s not exploding exponentially like it is in the US and Europe. Separately, the total number on the Y axis is in the tens, as opposed to the thousands. Again, there could be other factors at play, like Japan’s famously low-touch culture, with bows instead of handshakes.
However, even if we don’t have complete clarity on whether the use of masks is the driving factor in the success of numerous Asian countries in beating COVID-19, there’s another reason to do it…
This is an incredibly cheap thing to try
How much would it cost to give every American a set of five N95 masks to cycle through? According to a friend of mine who is sourcing masks for hospitals from reputable Chinese vendors, this would cost~$2.45 billion. If we went with surgical masks instead, this would cost ~$400 million. Masks aren’t that hard to make. Taiwan is making 10 million per day. China ramped from 20 million a day to 200 million a day in just two months. They could probably keep ramping up further if the US pushed to not just get enough for hospital workers, but enough for everyone.
In contrast, how much would a 3-month nationwide shutdown in Q2 cost the US? One analyst firm’s estimate predicts a 13% drop in GDP in Q2, which amounts to about $696 billion over 3 months. This actually sounds low to me as it may not be catching second order effects. As another way to measure things, public companies in the US have lost approximately $10 trillion in value over the last month. This doesn’t even count all the devastated small businesses. A general shutdown is clearly an expensive solution.
These options are starkly different. We could voluntarily do a really good job of taking individual action, wearing masks, washing our hands regularly, and immediately self-quarantining if we’re the least bit sick. Or we could shut everything down so people stay home and don’t infect one another. As a country that values individual liberty and the cowboy archetype of radical self-reliance, surely we’d choose the path where we’re all empowered to take action as opposed to the one where the government takes our freedoms away with a lockdown?
Fantastic Masks and How to Make Them
OK, by now I’ve hopefully convinced you that masks are worth considering. Now let’s get on to the details of how to make and use them.
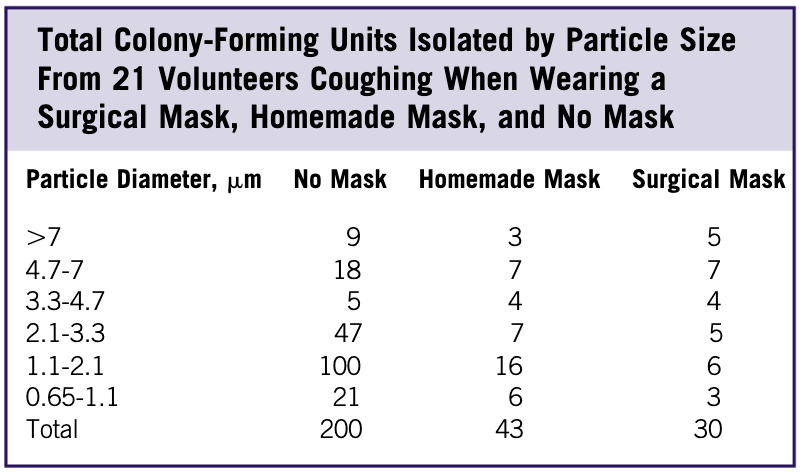
There have been several studies exploring the use of improvised masks in pandemics. One study looked at improvising masks using everything from vacuum cleaner bags to tea towels. There are tradeoffs between effectiveness and how easy it is to breathe through it. Antimicrobial pillowcases appear to be the best choice in this tradeoff, but many options exist. Even a basic cotton t-shirt cut the number of viruses in half.
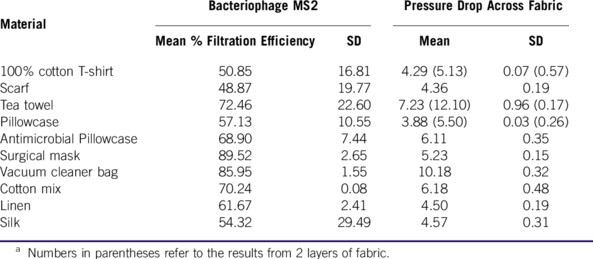
I should stress that these results are from a lab setting as opposed to a field setting. Actual function will depend on quality of fit.
Separately, the same study showed that homemade masks will dramatically reduce your probability of spreading your infection if you are sick or are infected but asymptomatic. Since you don’t know if you’re infected and asymptomatic, it’s definitely better to wear a mask as a precaution, even if it’s made from your old pillowcase.
Do you know how to sew and want to make your own mask? Here’s a tutorial. You might also be able to convince a friend who does know how to sew to make some for you.
Still too much work? Tie a bandana or a cut-up piece of a pillowcase over your nose and mouth, and you’re good to go. It’s not a great solution, but it’s something almost anyone can do in a few minutes. Try to make sure that the cloth sits out a bit from your mouth so that your lips are not making direct contact with it; when the mask becomes moist with droplets, you don’t want those droplets touching your lips.
It should be emphasized that cloth masks are considered a last resort in healthcare settings. They’re not nearly as effective as an N95 or a P100 respirator in virus-dense hospitals. However, they are a clear improvement over nothing when used by the general public so long as they are used and sanitized properly. They’ll also prevent you from touching your nose and lips, which is a major possible route for infection.
Go cut up that old pillow and make yourself a mask!
Proper use
There are plenty of guides to how to use a mask properly, but they come down to two basic things:
- Make sure you have a tight seal so air is actually going through the mask instead of around the sides. This makes a big difference.
- When you take it off, don’t touch the outside part; if the mask did catch any viruses, they’ll be on the outside. To be extra sure, wash or sanitize your hands before and after taking it off to prevent accidental contamination.
That was easy!
On to reuse!
As I mentioned, you’ll want to give most of your masks to healthcare workers and keep only a very small number for yourself. You’ll want to be able to use your mask again and again. There are several options for this.
Homemade fabric masks can be sterilized in boiling water and then dried fully. Alternately, they can be washed with detergent and hot (140F) water and then dried fully.
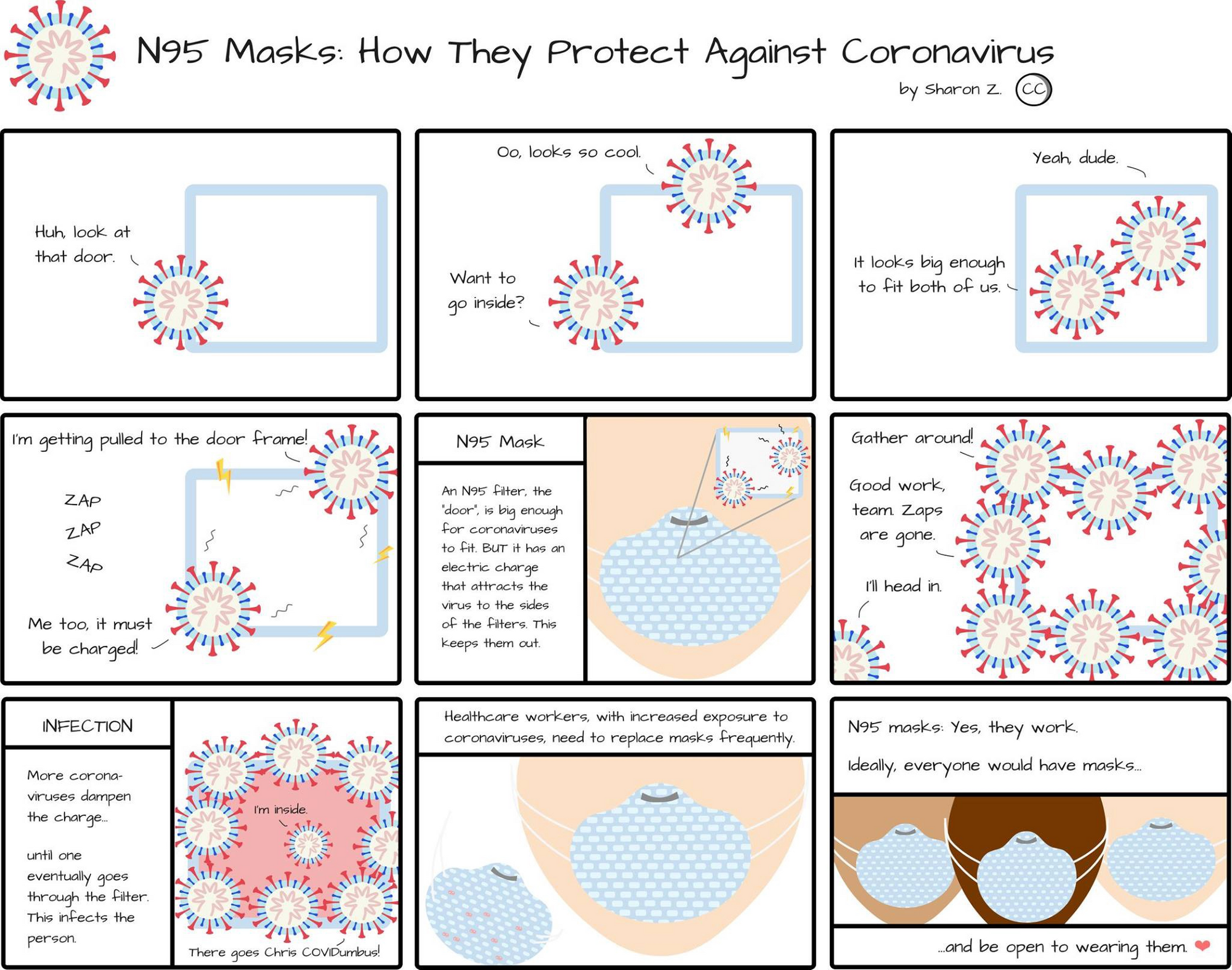
Reusing an N95 mask requires a different approach, which is laid out in this recent report by Stanford researchers. N95 masks work based on electrostatic attraction and need to stay dry. DO NOT wash N95s or use alcohol or bleach to clean them. This destroys the electrostatic attraction ability of the masks’ microfibers, and if you use bleach you might be breathing poisonous fumes that never quite go away. Most groups recommend discarding N95 masks once used in a high-risk setting (eg a hospital, or contact with a person with COVID-19) except as a last resort when supplies are running low. However, reuse after low-risk use appears to be possible and straightforward. An old study from SARS-CoV suggests that temperatures of 60C / 140F for 30 minutes will destroy this different coronavirus. There is no analogous study for the COVID-19 coronavirus yet, but it’s likely its temperature tolerance is similar. A recent study showed that N95 masks appear to only be mildly damaged by this level of heat. Thus, it’s possible you could “bake” your used N95 masks at low heat in the oven (eg 180F) to sterilize them without damaging them. I’ve tested this on the 3M brand N95 masks we have and it appeared to work — I use a temperature of 180F for 45 minutes to give some margin, as oven temperatures are not particularly accurate. The above study suggests that going significantly hotter than 180F may damage the mask.

It’s possible that multiple heating cycles may start to degrade the mask more substantially; this hasn’t been studied yet to my knowledge.
One alternative to heating the masks is to put them under a germicidal UV lamp for 30 minutes. This is apparently quite effective and does minimal damage to the mask. Some hospitals are starting to do this to deal with supply limitations. However, as a home user it may be difficult to make sure your UV lamp’s power is sufficient to penetrate through the mask and destroy the viruses, so heating may still be a safer option.
Yet another option is to simply let the masks sit in dry circulating air for at least 4 days to let the viruses degrade. This approach is advocated by Peter Tsai, the designer of N95 respirator technology, as an alternative if heating is unavailable.
Teach the Controversy!
The advice to wear masks in public is controversial in the US, and I’m going to try to address some of the common objections.
“The CDC told us not to wear masks”
I believe the CDC is trying to cover for the fact that they did not adequately stockpile masks for a pandemic, and now they don’t have enough for healthcare workers. They could have said “Hey, we messed up big time, and we need you all to make a small personal sacrifice so that the people who are putting their lives on the line are adequately protected. We’re going to make sure this never happens again, and we’ll get you all masks as soon as we can.” But instead they’re saying “The Centers for Disease Control and prevention does not recommend that well people wear a face mask to protect themselves from respiratory illnesses, including COVID-19”.
This is incredibly dangerous, as a recent NYT article points out, as it’s discrediting the idea of masks in general, which will make it harder to convince people to wear them in the future. It also ignores the possibility of creating makeshift masks.
Yes, let’s make sure that we get healthcare workers enough masks first, but in parallel we need to get everyone else wearing improvised masks, and then get them good ones once they’re available. We need to apply pressure to source an even larger number of masks, so that we have enough for healthcare workers AND delivery drivers AND grocery store cashiers AND the general public.
“You’re costing lives by not prioritizing healthcare workers”
I am prioritizing healthcare workers. As of this writing, hospitals will only take masks in their original packaging. If you have masks in their original packaging, donate them to a local hospital. There’s probably a mask drive in your area. However, if you have an open pack of masks, start using them. If you don’t, cut up that old pillowcase and make one!
“People don’t know how to wear them properly, and not wearing them properly just increases risk of infection”
We expect people to file their taxes, drive a car according to the rules of the road, etc. Surely we can teach the public how to wear a mask.
“The virus is smaller than the filter size of the mask”
It sure is! But that’s not how N95 masks work.
“If people think masks will protect them, they’ll go off and take risks which will make things worse”
This might be true for cloth masks, and it should be emphasized that cloth masks provide the least protection of any of the options listed here.
However, risk compensation is generally a strange line of argument, as it can lead to things like installing spikes in steering wheels to reduce the risk of car accidents. I don’t think we want to live in that world.
This isn’t the whole picture.
This goes without saying, but wearing a mask alone won’t protect you. You should be regularly washing/sanitizing your hands, coughing and sneezing into your elbow, avoiding physical contact with people other than intimate partners, avoiding crowds if at all possible, and quarantining yourself as soon as you feel sick. You should be teaching others to do the same.
At a policy level, we need to dramatically ramp up our testing capacity and start doing aggressive contact tracing of infected individuals. Contact tracing can be done manually or in a privacy-preserving automatic way, as we have seen Singapore do with their Bluetooth-based contact tracking app.
The more of these easy and cheap things we do, the fewer of the painful and expensive things we’ll have to do. This is up to us. We need to change norms about mask-wearing ASAP.
Thanks to Xianhang Zhang, Jeffrey Lin, and Jonathan Toomim for reading over drafts of this doc and making suggestions!
Originally published on Medium
