
Summary:
Sometimes the best solutions are the cheapest. The universal use of masks in public is one of the most cost-effective methods of stopping COVID-19. This is true even when the masks are simple cloth masks that people improvise from materials they have on hand. Multiple studies using different methodologies estimate that this intervention can result in a savings of $3,000-$6,000 for each person who starts wearing a mask, which is incredible for such a cheap intervention. The countries that have beaten back COVID-19 successfully have all made use of universal mask-wearing as a cultural practice, and there’s overwhelming evidence that universal mask-wearing in particular has a significant impact on curbing the spread of COVID-19.
When combined with extensive and proactive COVID-19 testing, contact tracing, isolation/quarantine, and public hygiene education, masks are an affordable part of a potent solution for stopping COVID-19 even in the absence of a vaccine or treatment. If we want to end the lockdown quickly, this combination of approaches is the most viable option.
How COVID-19 Spreads:
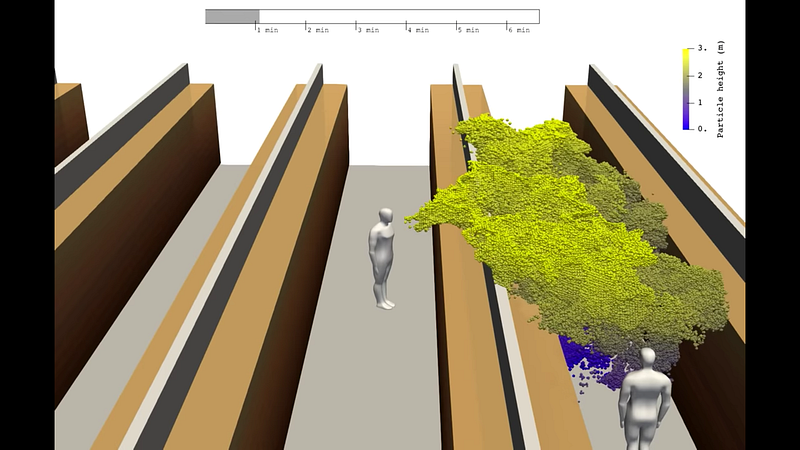
Researchers believe that COVID-19 is primarily spread through respiratory droplets and contact with shared surfaces. As an infected person breathes, speaks, or coughs, they exhale small droplets of water containing viruses. Other people nearby can inhale these invisible droplets. The risk of this happening is higher in enclosed spaces as well as in more crowded spaces. In general these droplets tend to travel a maximum of around 2 meters in calm conditions, gradually settling onto the ground or other surfaces. However, some droplets are small enough that they remain airborne for longer. These smaller droplets are called aerosols. There is evidence that other coronaviruses are present in exhaled aerosols, which means there is a chance that SARS-CoV-2 may be present in the aerosols exhaled by infected individuals as well. Internal airflow and ventilation systems may cause these aerosols to travel further, as a recent study shows. Another study of a hospital in Wuhan found samples of SARS-CoV-2 on the surfaces of vents and in the air up to 4 meters away from patients, lending further credence to the possibility that the virus can spread in aerosols. Thus, simple social distancing may be inadequate to stop the spread of COVID-19.
If you can stop virus-bearing droplets from entering a person’s mouth, nose, or eyes, you prevent them from being infected. If you can stop these droplets from leaving an infected person’s mouth, you prevent them from infecting others. Respirator masks (e.g. N95s) help with both of these tasks, while surgical masks and cloth masks primarily help with the latter. While masks are not perfect, they are able to dramatically reduce the transmitted or received viral load, which reduces the risk of infection. Masks also have the added benefit of preventing people from touching their nose and mouth with dirty hands, which is another common route of infection.
In a hypothetical, ideal world in which everyone wears a top-quality respirator mask continuously and practices careful personal hygiene, COVID-19 would have a very difficult time spreading from person to person, and would quickly die out. However, even assuming realistic use conditions and reliability, a recent correlational study estimates a $3,000-$6,000 benefit from each additional cloth mask worn by members of the public during the COVID-19 pandemic, with a much higher benefit per mask for higher-end masks worn by healthcare workers in high risk settings.
There is clear indication that even improvised cloth masks can have a significant impact on the spread of COVID-19 so long as adherence is high. Fortunately, public adherence does not appear to be a problem. Even countries such as the United States that have no history of mask-wearing in public (and a president who declares that he will not wear one) now see over half of people wearing masks as of April 9th.
This article will dive into the evidence for the effectiveness of masks in fighting COVID-19, the range of masks available, and how limited supply can be overcome.
Masks and Reproduction Number
The reproduction number, or “R”, of an infectious disease, is the number of individuals that an infected individual infects on average. If R is above one, the infection grows exponentially and spreads throughout the population. If R is below one, the infection shrinks and ultimately disappears. Estimates of the R0 (the reproduction number if no countermeasures are taken) of COVID-19 vary significantly, but most of them are above 2. All of the countermeasures being contemplated, from social distancing to business closures to masks, have an impact on the value of R.
One of the things that has made COVID-19 so difficult to fight is that infected individuals can spread the disease before any symptoms appear. One study concluded that the reproduction number of COVID-19 is about 1 from asymptomatic and presymptomatic carriers alone, which means that it’s very difficult to stop the disease unless individuals who appear healthy start wearing masks. From the aforementioned study, here’s a graph of how many days after infection that various types of contagion happen. While testing at the first sign of symptoms is very effective for identifying symptomatic individuals, masks are also able to put a dent in presymptomatic and asymptomatic transmission.
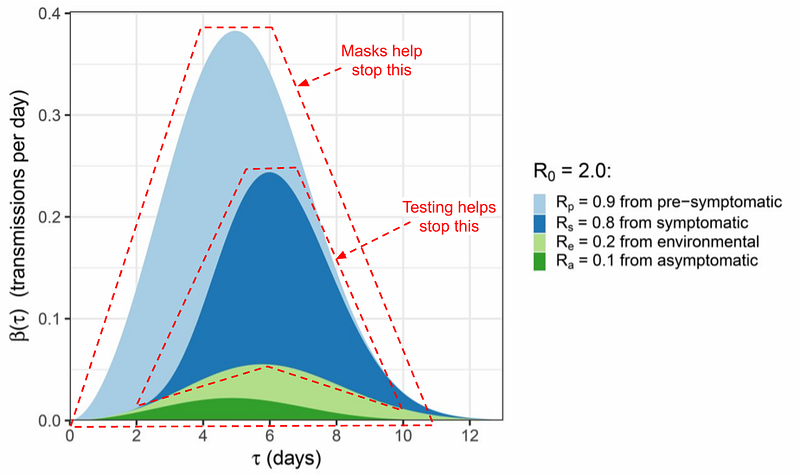
Given that masks can play a significant role in reducing all types of transmission of the virus, even an imperfect mask that only catches a fraction of the viruses passing through it can still have a very significant impact on R.
Studying Mask Effectiveness
How do we know how well masks work? Here are three ways we’ll explore:
- Country-by-country comparison of COVID-19 strategies
- Lab analysis of mask materials
- Controlled trials of masks for preventing influenza
Country-by-country comparison of COVID-19 strategies
It’s very tricky to do a definitive factor analysis of different countries’ COVID-19 outbreaks. There can be thousands of factors that explain why one country is doing better than another. We will try to control for extraneous variables to the extent it’s possible to do so, and do the best we can at teasing out the effect of masks in particular. We will also look at evidence of the effects of mask-wearing in five different ways.
Country Evidence Part 1: The SARS survivors
Nearly every Asian public health ministry recommends that people wear masks in public, especially during the winter flu season. Japan, Hong Kong, South Korea, and Taiwan all recommend wearing masks, and all of these countries have been effective in slowing the spread of COVID-19 within their borders without having to resort to Wuhan-style lockdowns.
This is such a huge deal that it bears repeating. Daily life in Japan, Hong Kong, South Korea and Taiwan is only slightly affected. Some large gatherings are prohibited and some schools are closed, but life on the street goes on. Stores, restaurants, and most other businesses are open. What do these countries have in common? They all were affected by the SARS epidemic in 2003. When news of COVID-19 broke, everyone put on masks and started sanitizing or washing their hands every time they entered an office or restaurant. This rapid action happened at both the individual level and at the national level. Taiwan in particular had an almost immediate response that involved nationwide requisition and distribution of masks to hospitals and to the general public almost as soon as the Wuhan lockdown happened. Taiwan managed to cap its total cases at 382 (as of 4/10/20) despite the enormous number of people traveling daily to and from China when the outbreak occurred.
You can see that these countries all performed quite well relative to the rest of the world, despite being the initial areas of the outbreak:
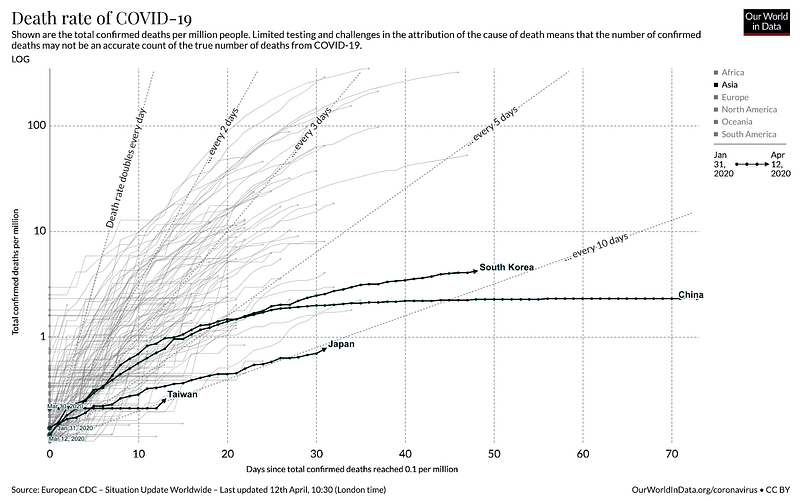
Of these countries, only Japan’s outbreak is still sizable and growing, but it’s worth noting that they have been rather slow and reactive with regard to testing or any other countermeasures, with the exception of closing schools.
However, this evidence is not sufficient to conclude that masks were the deciding factor as there may be other cultural factors at play. These cultures tend to be lower-touch than Western cultures, in many cases with bowing replacing handshakes. Reduced touch makes it much harder for the virus to spread. Separately, differences between more individualist and collectivist cultures may play a role as well, with residents of collectivist cultures more willing to take individually inconvenient actions for the common good.
Country Evidence Part 2: What happens if you ONLY use Masks?
While Japan has not had as proactive of a response to COVID-19 as other Asian countries, their caseload does provide an interesting window into the possible effect of masks in particular to reduce COVID-19 transmission. Japan gives us a sense of what happens in a dense country that does little to combat community spread of COVID-19 except encourage people to start wearing masks. We can compare the rate of spread in Japan to the rate of spread in countries that pre-lockdown had similar policies to Japan in terms of immigration restrictions but did not encourage the wearing of masks.
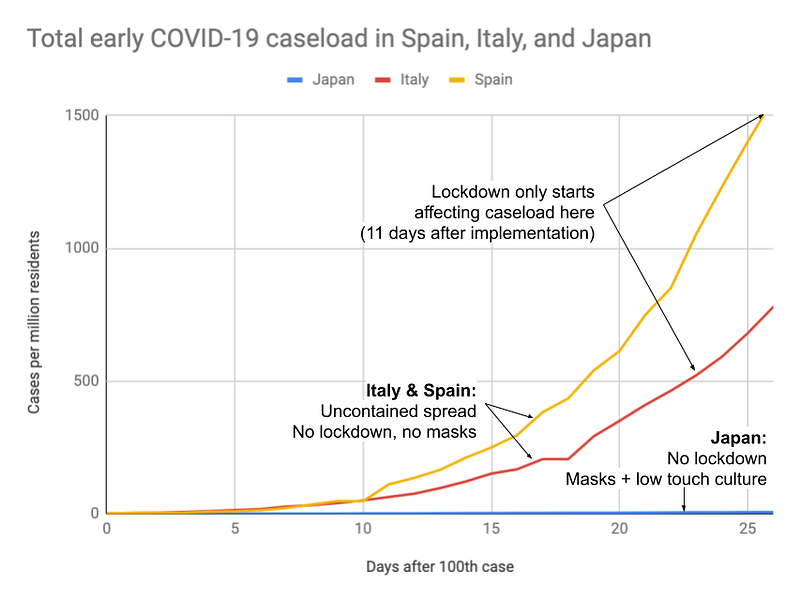
Even another month past the right end of the graph and despite doing very little to fight COVID-19, Japan’s case growth rate is still slow, with a doubling time of 6.6 days over the past week (as of 4/10/20), compared with the doubling time of 2–3 days seen during uncontained growth in Spain, Italy, and other places.
As in Part 1, it’s still unclear whether masks or other cultural factors are the primary influence, but we’ll get other chances to look at this evidence.
Country Evidence Part 3: Combining masks, testing, tracing and isolation
Next, we’ll turn to South Korea, one of the few countries that got everything right. South Korea is using masks in conjunction with other interventions to successfully beat COVID-19. They are doing an excellent job of tracing the contacts of everyone who might have been infected and aggressively testing them to encircle any outbreaks that are happening. This coherent strategy is undoubtedly vital to controlling the spread of the disease.
Let’s compare South Korea to the US.
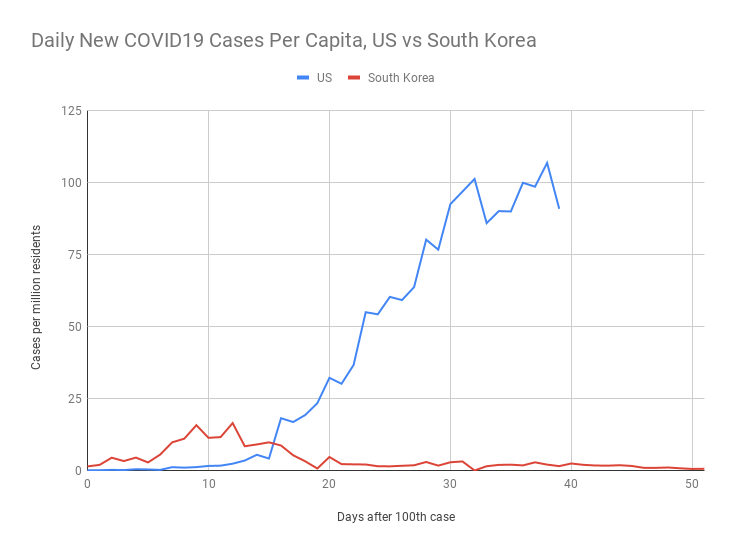
South Korea had an initial spike in cases driven by a handful of super-spreader events in a church, but was quickly able to react and get it under control. The country shut down a handful of locations of known outbreaks, but did not enact a general shelter-in-place order. The people of South Korea, remembering the SARS epidemic, did take some voluntary measures to avoid crowded places in areas where outbreaks happened.
In comparison, most of the US has enacted business closures and shelter-in-place orders, but has not pushed to make the wearing of facemasks mandatory, and lags far behind South Korea in terms of testing and contact tracing.
It’s clear that the combination of measures that South Korea enacted worked to quell an explosion of cases, but this is insufficient evidence to point towards masks in particular being the deciding factor. To study that, we will have to find a case where multiple countries took similar measures but some took the additional step of requiring facemasks.
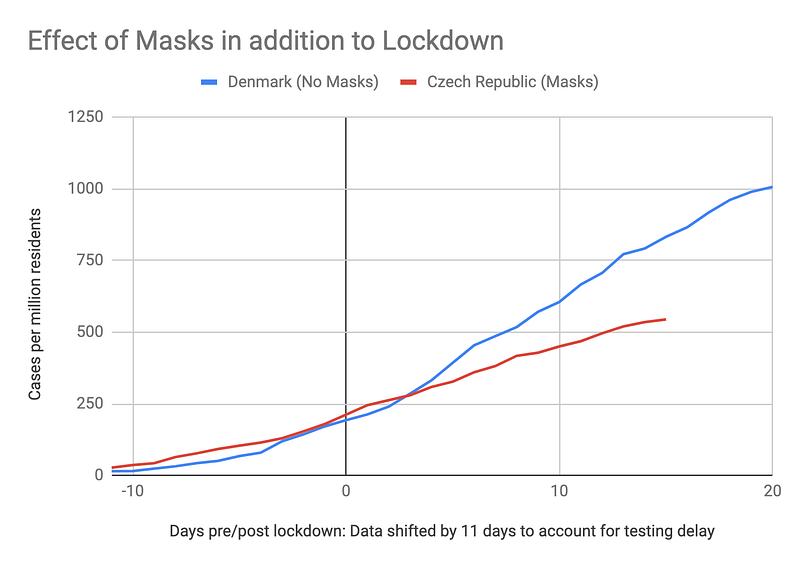
Country Evidence Part 4: Examining the addition of masks to lockdown
The best assessment of mask use would be a proper side by side comparison of otherwise similar countries with similar cultures and demographics. Fortunately, this comparison exists. In Europe, most countries enacted shelter-in-place between March 9th and March 25th.
However, two countries, the Czech Republic and Slovakia, chose to take the additional step of requiring all residents to wear masks. Slovakia started requiring masks in shops and on public transport on March 15th (as well as outdoors on March 24th), and the Czech Republic started requiring masks in all indoor and outdoor public locations on March 18th. In general it takes around 11 days for policy changes to show up in a difference in COVID tests unless there is a robust South Korea style test + contact tracing program in place. Thus, if we look at the growth rate in cases during the last 10 days (April 1st to April 11th) we will be able to see the effect of policy decisions before March 20th.
This allows us to isolate the effect of universal mask-wearing among a set of countries that have all entered shelter-in-place.
In order to ensure a fair comparison, we made the following restrictions when comparing countries:
- To ensure that the case growth trendline represents the effect of lockdown, countries that locked down after 3/20 are excluded. Since the effect of lockdown may take 11 days to show up, the period 4/1–4/11 entirely represents the case growth during lockdown
- Countries with fewer than 5 million residents are excluded as case counts are sometimes too small for trend analysis
- Different countries are more and less aggressive with testing, which also has a significant effect on the rate at which the disease spreads. Both countries with limited testing (less than 10 tests per COVID case) and extensive testing (more than 10 tests per COVID case) are included here.

The effect is surprisingly strong. The countries that have implemented mask-wearing have lower caseloads and lower growth rates than the countries that did not. For example, Slovakia (in red) is at the bottom left of the chart, with decreasing growth in new cases (x-axis) and a low number of active cases per million residents (y-axis) as of April 11. Czechia is in a similar situation. They’re not the richest countries in Europe, but they have managed to find a low-cost way of keeping their countries safe.
Country Evidence Part 5: A deep dive on two European countries
To further note the difference between masks vs no masks, we’re going to compare the Czech Republic to another country with very similar circumstances, Denmark. Both countries were in a relatively similar position at the time of lockdown (similar population density, ample testing, similar caseload per capita, similar lockdown dates) but only the Czech Republic took the additional step of requiring masks, so we can see how the two countries diverged.
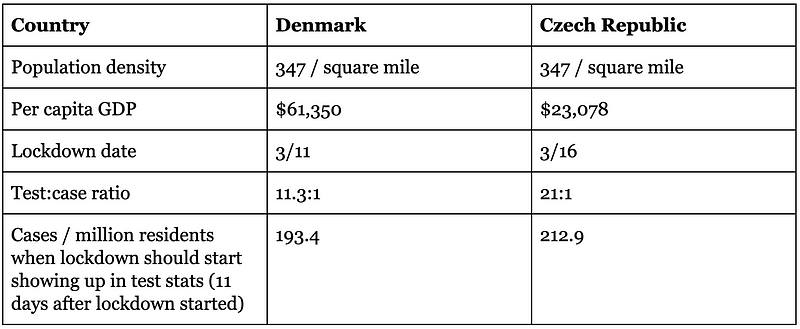
Comparisons of single countries must be done carefully as there can be many additional factors that may be coming into play, but it does appear that the Czech republic fared substantially better than Denmark despite being a poorer country.
Lab analysis of mask materials
Next, we will examine studies of the role of masks in stopping inhalation of particles. To do so, we’ll need to go on a brief diversion into the range of masks available.
Many types of masks have been created for a range of applications from construction to mining to factory work to medicine. As we’ll show, any of these masks will convey some benefit over no mask at all, so long as they are handled properly. These masks are arranged in the following table in roughly decreasing order of effectiveness.
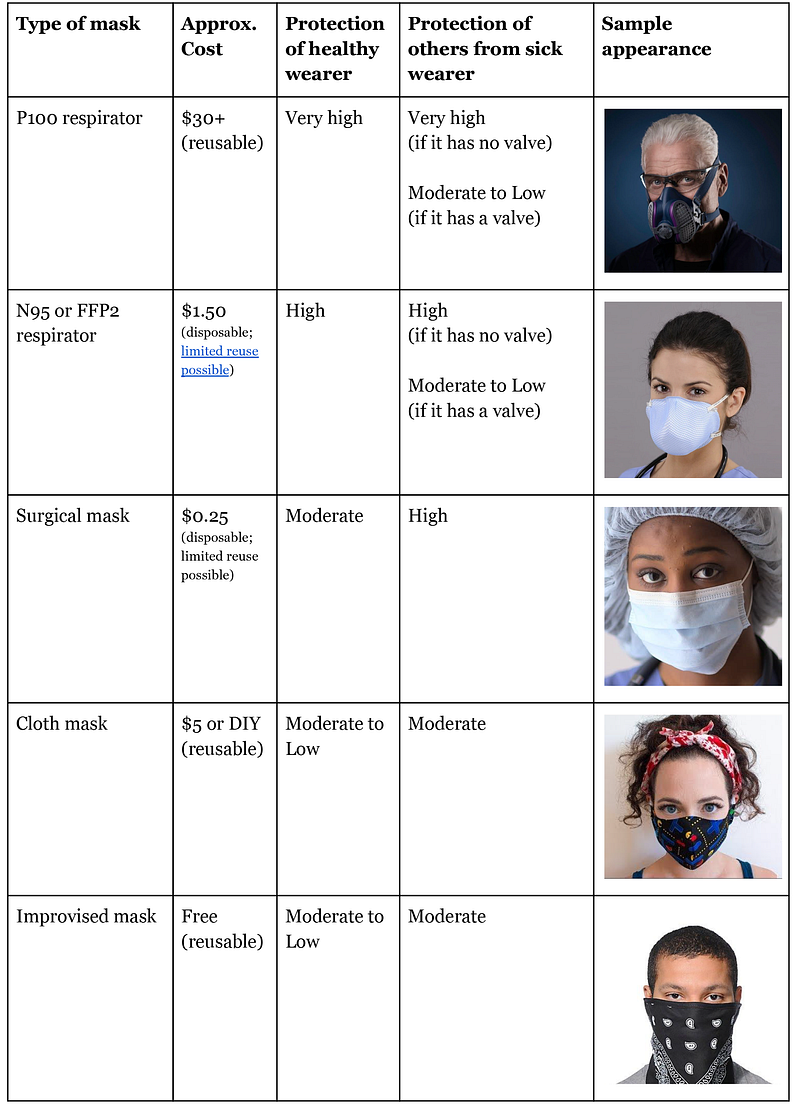
In a supply-limited scenario it makes sense for governments to reserve the highest quality masks for healthcare workers and other people in high-exposure scenarios (eg public transit workers, store clerks) while providing a rationed number of inexpensive masks to the public or encouraging the public to get whatever masks they can, improvising if necessary, and educating them in how to use them properly. It’s worth emphasizing that even an improvised mask is significantly better than no mask.
Mask filtration efficiency
A P100 respirator, by definition, stops at least 99.97% of particles down to 0.3 microns. An N95 respirator, by definition, stops at least 95% of particles down to 0.3 microns. Both these respirators are widely used in healthcare settings in which healthcare workers are in prolonged contact with highly contagious COVID-19 patients. Surgical masks offer somewhat lower protection and are considered inadequate protection from COVID-19 in healthcare settings, though they are still used in COVID-19 treatment wards due to supply issues.
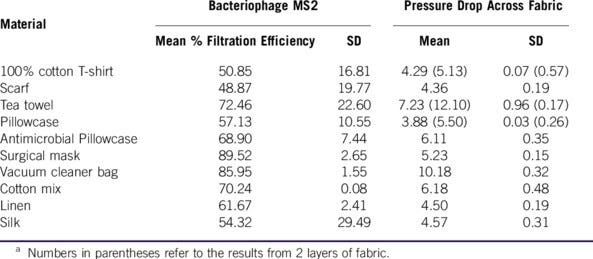
For general public use, there have been several studies exploring the use of improvised masks in pandemics. One study looked at improvising masks using everything from vacuum cleaner bags to tea towels, and compared them to the performance of surgical masks. Note that several materials performed nearly as well as a surgical mask. There are tradeoffs between the effectiveness of a mask and how easy it is to breathe through it. Antimicrobial pillowcases appear to be the best choice in this tradeoff, but many options exist. Even a basic cotton t-shirt cuts the number of viruses passing through the material in half. A cautionary note — while vacuum cleaner bags are the most effective option, several people have raised the concern that microfiber shards in the vacuum cleaner bag could cause their own health issues if inhaled, so that option should probably be avoided.
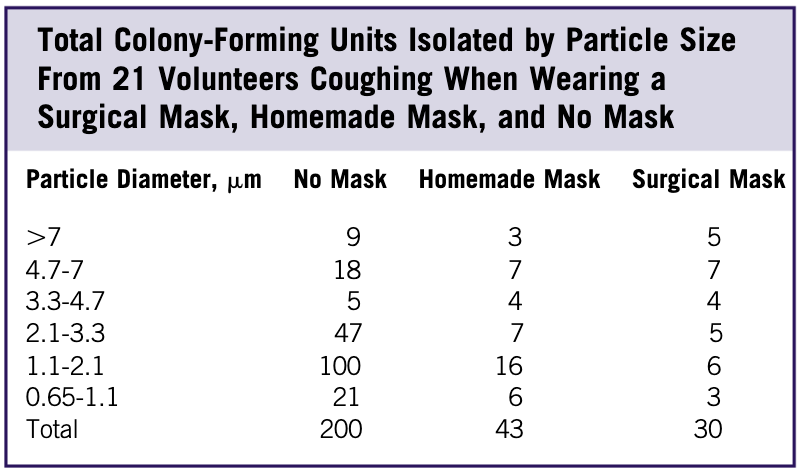
Next, we’ll examine the role of masks in stopping an infected person from spreading their illness. One study showed that homemade cloth masks will dramatically reduce your probability of spreading your infection if you are sick or are infected but asymptomatic. In fact, homemade cloth masks perform almost as well at stopping droplets as surgical masks. This is a huge deal, as it’s much easier to give people instructions in improvising masks than it is to procure surgical masks for everyone. In the table below, homemade and surgical masks are compared against no mask in terms of the number of bacteria-containing droplets of various sizes exhaled by a person coughing. There’s a massive reduction in droplets from the use of both types of masks.
The impacts of even a homemade mask are very dramatic. A second study highlighting the effect of speech on droplet formation as well as the effect of cloth masks on blocking their transmission corroborates these results.
However, it would be even better to directly measure the viral load that is carried through the mask worn by a contagious individual. While the above studies do not do that, another study using a different coronavirus (not SARS-CoV-2) shows that the viral load detected in exhaled droplets and aerosols is dramatically reduced by the use of a surgical mask.
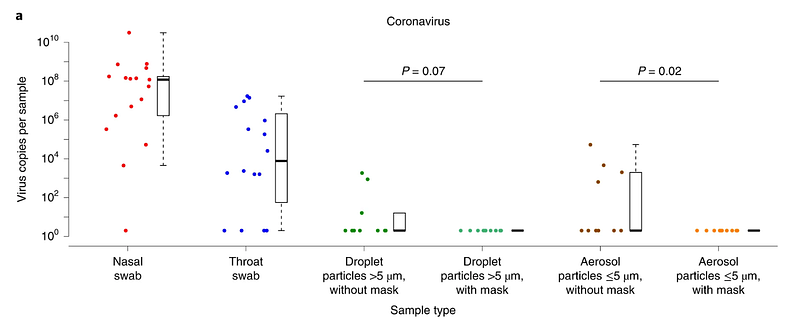
Given that droplet transmission is dramatically reduced by cloth masks and surgical masks, and transmission of other coronaviruses is dramatically reduced by surgical masks, it’s reasonable to conclude that even cloth masks might significantly reduce the spread of COVID-19.
Controlled trials of masks for preventing influenza
There have been many studies on respirators and masks in healthcare settings as well as home settings in which a family member is sick. Most of these studies examined the effect of masks on the spread of regular influenza during flu season. This 2015 review of the literature provides a good overview. Studies on the protectiveness of masks in real-world settings are complicated to do and confounded by other factors, but there is strong evidence that masks are useful in healthcare settings and decent evidence that masks are useful in home settings.
From this, it’s possible to extrapolate that masks would likely be helpful in a pandemic setting. One challenge of home setting studies is that they are particularly difficult to show effectiveness. These studies require participants to wear masks at all times while at home with a sick relative. Relatively few people are able to adhere to this protocol, which is more challenging than wearing a mask when going out. Separately, adherence is much higher in a pandemic due to fear; people are much more afraid of catching a disease during a pandemic than they are afraid of catching a regular flu during a study. Thus, we should expect that people would wear masks much more reliably in a pandemic setting than in a home study setting. This means the results of mask use in a pandemic setting will likely be better than they are in a home setting, and these results were already decently good in a home setting.
Furthermore, there is some evidence that masks may be more protective with coronaviruses than with influenza viruses, which would further point toward the usefulness of wearing a mask in the current pandemic.
Challenges
There are a handful of challenges in implementing a national requirement for use of masks, but none of them are particularly insurmountable.
Supply
While countries such as Taiwan have a national stockpile of masks in case of a pandemic, most Western countries do not. This has created a global rush to procure a limited supply of masks, with predictable issues of price-gouging, subpar goods, counterfeiting, and bureaucratic infighting around the acceptance of different mask standards in different countries. Mask suppliers are drastically increasing production to meet demand, but this will take time.
While procurement of high-quality masks for healthcare workers is a serious issue and is out of scope of this analysis, the use of improvised masks by the general public can get around supply issues in the short term. The Czech Republic has shown it’s possible to get all residents to sew or improvise cloth masks in the space of a week. Furthermore, there are a number of methods for reusing masks that can help extend limited supply. Finally, the government can play a role in procuring and rationing masks to ensure that all residents have an adequate supply.
Education:
Educating the public in proper use of masks is straightforward but important to get right. There are plenty of guides to how to use a mask properly, but they come down to some basic things:
- Make sure there is a tight seal so air is actually going through the mask instead of around the sides. This makes a big difference.
- Mask-wearers need to make sure that they do not touch the mask while wearing it, as well as resist the impulse to reach under the mask to scratch an itch.
- When the wearer takes the mask off, they need to immediately wash or sanitize their hands. If the mask caught any viruses from the outside world, they’ll be on the outside. If the wearer is infected and contagious, there will be viruses on the inside of the mask. In either case, touching the mask makes the person’s hands potentially contaminated, and they should wash or sanitize them immediately.
- Masks need to be sterilized or discarded after each use.
The Czech government accomplished this public education with a PSA (summarized here) that was shared with residents. The US’s CDC has a set of guidelines on both the construction and proper use of cloth masks.
Reuse
Reuse of cloth masks is relatively simple. They can be sterilized in boiling water and then dried fully. Alternately, they can be washed with detergent and hot (140F) water and then dried fully.
Washing does not work on N95 masks as it destroys their electrostatic attraction, which is how these masks are able to trap particles far smaller than the size of the holes in the mask. Instead, N95 masks used by the general public in lower-risk settings can be “baked” in an oven at a temperature of ~180F for at least 30 minutes to kill off the virus. Alternately, masks may simply be left to sit in dry circulating air for at least 4 days to let the viruses degrade, though another study on surgical masks suggests that some viral load may still be present after 7 days. For hospital-grade reuse after use in higher-risk settings, there are a number of additional options, as laid out in this recent report by Stanford researchers. A recent study shows that N95 masks gradually degrade with multiple rounds of sterilization and reuse, and 2 sterilization cycles should be the limit.
Conflicting messaging
Despite clear evidence for their effectiveness, there has been conflicting messaging around the effectiveness of masks. Until recently, the US’s CDC specifically recommended that the general public not wear masks. They now cautiously recommend the use of cloth masks. The WHO still does not recommend the use of face masks by the general public unless they are sick.
In both cases, the recommendation may likely have been driven by a concern that members of the public would be competing with healthcare workers for masks, and healthcare workers are higher priority.
Fortunately, cloth masks are not subject to these supply limitations, allowing members of the general public to start wearing them immediately while supplies ramp up.
Risk compensation
Public health officials at the WHO and CDC have expressed a concern that people will overestimate the protective effects of masks, leading them to neglect social distancing or otherwise increase their risk profile in a way that increases overall risk. This has proven not to be true in other scenarios such as motorcycling and adventure sports, in which use of helmets has resulted in a net decrease in injuries. It also appears to not be true in the case of COVID-19 as well given the data we are seeing.
Resistance to habit change
Unlike in Asia, there is a stigma on mask-wearing in most Western cultures, where a someone with a mask is either regarded as infectious or pathologically germophobic. Fortunately, in the face of a deadly pandemic, this seems to not be as much of an issue. 55% of Americans now wear a mask out in public according to a recent poll.
Opinions around the world are wildly divergent but tilting toward increased public interest in wearing masks. It’s impressive how quickly public behavior can change in the span of a month, but most countries still have a ways to go to reach full adoption of masks.
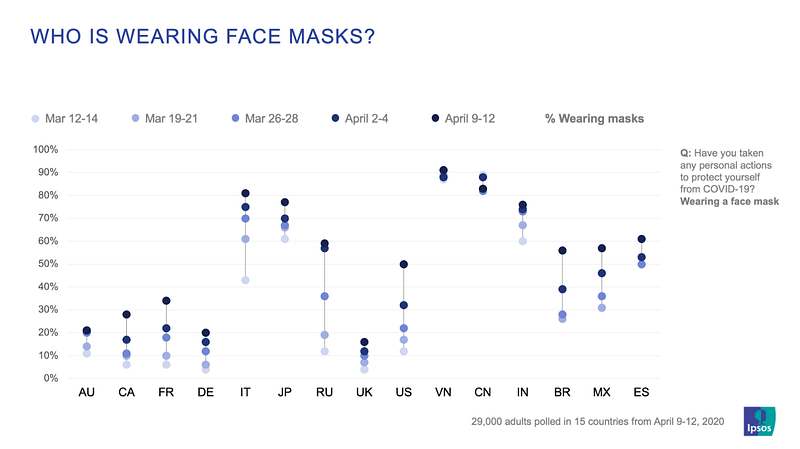
Of particular note is Vietnam, where adherence to mask wearing has been close to 90% over the last month. Vietnam is not a wealthy country (per capita GDP $2,566) but their government was very proactive in public education around hygiene and masks, even going so far as to release a catchy educational song and music video on February 23rd. Their total COVID-19 caseload never exceeded 300, and they are seeing only a handful of new cases a day.

Cost-Effectiveness
The cost of rolling out a national requirement for cloth masks is very low — it’s simply the cost of a PR campaign that would be amplified for free by national media.
If we set our sights higher, how much would it cost for the US to give every resident a set of five N95 masks to cycle through? According to someone who is sourcing masks for hospitals from reputable Chinese vendors, this would cost~$2.45 billion. If the US distributed surgical masks instead, this would cost ~$400 million. Masks can be made in tremendous quantities. Taiwan is making 10 million per day. China ramped from 20 million a day to 200 million a day in two months. With more time and continued demand, factories around the world could ramp up further.
A recent correlational study estimates a $3000-$6000 benefit from each additional cloth mask worn by members of the public during COVID-19. At the scale of the United states, that would translate to a $1-$2 trillion benefit. Another study done on a hypothetical H1N1 pandemic estimated a savings of $573 billion if just half of America were supplied with a set of N95 masks — this translates to a roughly $3500 benefit per person. Although these studies used radically different methodologies to arrive at their numbers, they both point toward a very clear argument for the cost-effectiveness of universal mask wearing. The cost of doing so is several orders of magnitude better than shelter-in-place measures.
Key Performance Indicators
In order to evaluate how well a country or region is doing with mask use, the following KPIs are advisable:
- % of public that is voluntarily wearing masks of some sort
- Active encouragement by national health authorities toward universal wearing of masks
- National order requiring the universal wearing of masks
- Sufficient supply of N95 masks or equivalent for healthcare workers
- [Stretch goal] Sufficient supply of N95 masks or equivalent for the general public
Examination of how countries are performing against these KPIs will help further study of the effectiveness of masks.
Follow-up and Help
If you have connections to policy-makers at the national, state, or local levels, please share this document with them. Leaders in major cities including New York, Austin, and Los Angeles are starting the shift toward requiring the public to wear masks in the US, and we’re excited to see the movement spread. Separately, if you are in a culturally influential position to encourage new norms around mask-wearing, help get the message out!
Further Reading
A comprehensive literature review of the effectiveness of masks in fighting COVID-19 has recently been published and is highly recommended as a next step for understanding the effectiveness of masks in further detail.
Acknowledgements
Thanks to everyone who read over this article and provided feedback, including Genevieve Gee, Christina Müller, Tomas Pueyo, Christine Gibson, Joe Vipond, Carl Juneau, and Lydia Laurenson!
This post was originally published on Medium.
